Three people with severely impaired vision who received stem-cell transplants have experienced substantial improvements in their sight that have persisted for more than a year. A fourth person with severely impaired vision also experienced gains in their sight, but they did not last. The four are the first to receive transplants made from reprogrammed stem cells to treat damaged corneas, the transparent outer surface of the eye1.
The results, described in The Lancet today, are impressive, says Kapil Bharti, a translational stem-cell researcher at the US National Eye Institute, National Institutes of Health, in Bethesda, Maryland. “This is an exciting development.”
“The results merit treating more patients,” says stem-cell researcher Jeanne Loring at Scripps Research in La Jolla, California.
Reprogrammed cells
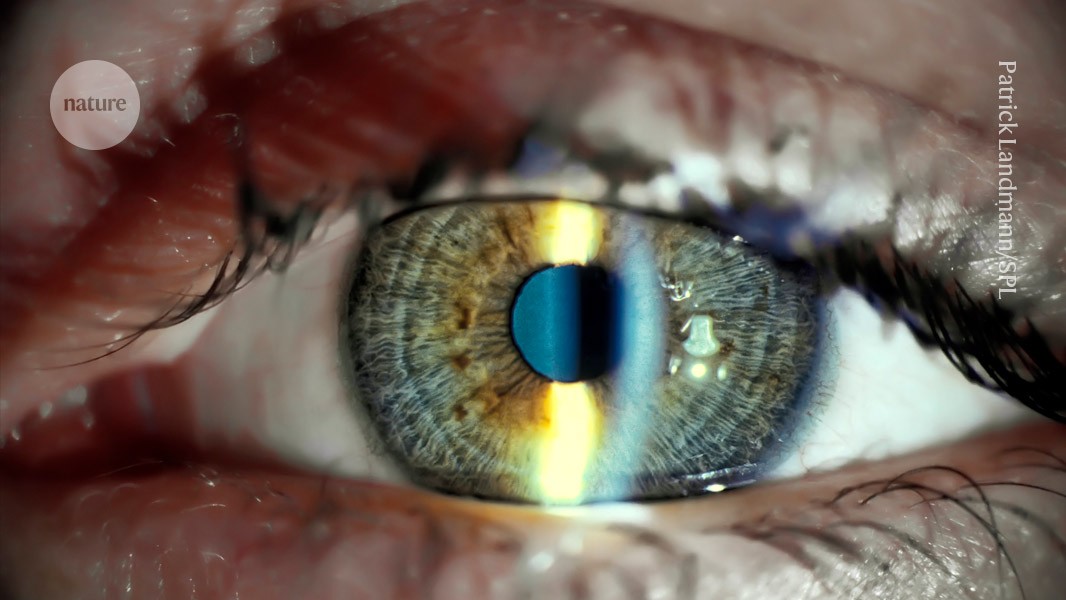
The outermost layer of the cornea is maintained by a reservoir of stem cells housed in the limbal ring — the dark ring around the iris. When this essential source of rejuvenation is depleted — a condition known as limbal stem-cell deficiency (LSCD) — scar tissue coats the cornea, eventually leading to blindness. It can result from trauma to the eye or from autoimmune and genetic diseases.
Treatments for LSCD are limited. They typically involve transplanting corneal cells derived from stem cells obtained from a person’s healthy eye, which is an invasive procedure with uncertain outcomes. When both eyes are affected, corneal transplants from deceased donors are an option, but these are sometimes rejected by the recipient’s immune system.
Kohji Nishida, an ophthalmologist at Osaka University in Japan, and his colleagues used an alternative source of cells — induced pluripotent stem (iPS) cells — to make the corneal transplants. They took blood cells from a healthy donor and reprogrammed them into an embryonic-like state, then transformed them into a thin, transparent sheet of cobblestone-shaped corneal epithelial cells.
Between June 2019 and November 2020, the team enrolled two women and two men aged between 39 and 72 years old with LSCD in both eyes. As part of the surgery, the team scraped off the layer of scar tissue covering the damaged cornea in only one eye, then stitched on epithelial sheets derived from a donor and placed a soft protective contact lens on top.
Vision test
Two years after receiving the transplants, none of the recipients had experienced severe side effects. The grafts did not form tumours — a known risk of growing iPS cells — and did not show clear signs of being attacked by the recipients’ immune systems, even in two patients who did not receive immunosuppressant drugs. “It is important and a relief to see grafts were not rejected,” says Bharti. But more transplants are needed to be certain of the intervention’s safety, he says.
After the transplants, all four recipients showed immediate improvements in their vision, and a reduction in the area of the cornea affected by LSCD. The improvements persisted in all but one recipient, who showed slight reversals during a one-year observation period.
Bharti says it isn’t clear what exactly caused the vision improvements. It’s possible that the transplanted cells themselves proliferated in the recipient’s corneas. But the vision gains could also be due to the removal of scar tissue before the transplant, or the transplant triggering the recipient’s own cells to migrate from other regions of the eye and rejuvenate the cornea.
Nishida says they plan to launch clinical trials in March, which would assess the treatment’s efficacy. Several other iPS-cell-based trials are under way globally to treat eye diseases, says Bharti. “These success stories suggest we are headed in the right direction.”