
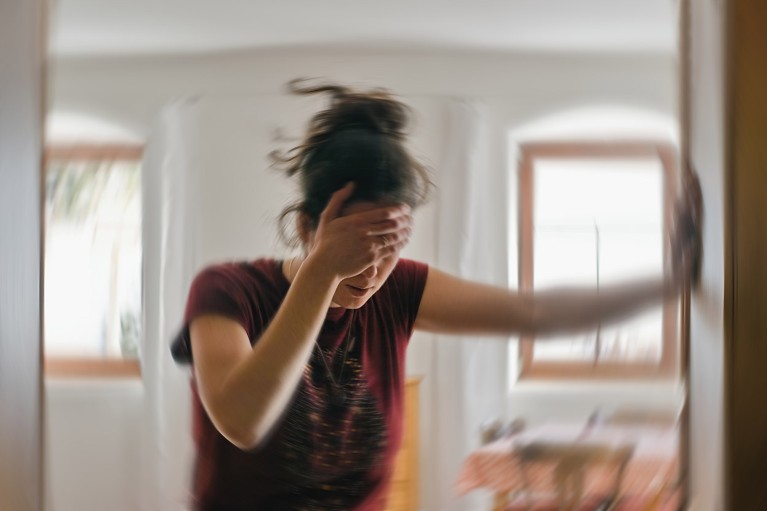
About one-third of people who suffer from migraines experience a phenomenon known as aura before the headache.Credit: Tunatura/Getty
For a billion people worldwide, the symptoms can be debilitating: throbbing head pain, nausea, blurred vision and fatigue that can last for days. But how brain activity triggers these severest of headaches — migraines — has long puzzled scientists.
A study1 in mice, published in Science on 4 July, now offers clues about the neurological events that spark migraines. It suggests that a brief brain ‘blackout’ — when neuronal activity shuts down — temporarily changes the content of the cerebrospinal fluid, the clear liquid that surrounds the brain and spinal cord. This altered fluid, researchers suggest, travels through a previously unknown gap in anatomy to nerves in the skull where it activates pain and inflammatory receptors, causing headaches.
“This work is a shift in how we think the headaches originate,” says Gregory Dussor, a neuroscientist at the University of Texas at Dallas in Richardson. “A headache might just be a general warning sign for lots of things happening inside the brain that aren’t normal.”
“Migraine is actually protective in that way. The pain is protective because it’s telling the person to rest and recover and sleep,” says study co-author Maiken Nedergaard, a neuroscientist at the University of Copenhagen.
No-pain brain
The brain itself has no pain receptors; the sensation of headaches comes from areas outside the brain that are in the peripheral nervous system. But how the brain, which is not directly linked to the peripheral nervous system, triggers nerves to cause headaches is poorly understood, making them difficult to treat.
Scientists working with a mouse model of a particular type of headache, called aural migraine, set out to explore this. One-third of migraine sufferers experience a phase before their headache known as aura that has symptoms such as nausea, vomiting, sensitivity to light and numbness. It can last five minutes to an hour. During aura, the brain experiences a blackout called a cortical spreading depression (CSD), when neuronal activity shuts down for a short time.
Studies of migraines have suggested that headaches happens when molecules in the cerebrospinal fluid drain from the brain and activate nerves in the meninges, the layers that protect the brain and spinal cord.
Nedergaard’s team wanted to explore whether there are similar leaks in the cerebrospinal fluid that activate the trigeminal nerve, which runs through the face and skull. The nerve branches join at the trigeminal ganglia at the base of the skull. This is a hub for relaying sensory information between the face and jaw to the brain, and contains receptors for pain and inflammatory proteins.
Nerve bundle
The authors bred mice that experienced CSDs and analysed the movement and content of their cerebrospinal fluid. During a CSD, they found that the concentrations of some proteins in the fluid dropped to less than half their usual levels. The levels of other proteins more than doubled, including that of the pain-transmitting protein CGRP, which is one target of migraine medications.
The researchers also discovered a previously unknown gap in the protective layers around the trigeminal ganglion, which allows cerebrospinal fluid to flood into these nerve cells. So they tested whether spinal fluids with different protein concentrations activated the trigeminal nerves in control mice.
Fluid collected shortly after a CSD increased activity of trigeminal nerve cells — indicating that headaches could be triggered from pain signals sent from these activated cells. But the fluid collected 2.5 hours after CSDs didn’t have the same effect.
“Whatever is released in the cerebrospinal fluid is degraded. So, it’s a short-lasting phenomenon,” says Nedergaard.
“It really shows this nice potential interaction between how something changing in the brain could impact the periphery. There can be a crosstalk between these two components of the nervous system, and we should be more aware of it,” says Philip Holland, a neuroscientist at King’s College London.
Dussor suggests that future studies should explore why the proteins in spinal fluid that hit the trigeminal ganglion result in headaches and no other type of pain. “This is going to raise a whole lot of interesting questions in the field, and it’s going to be probably the source of a lot of new research projects.”

