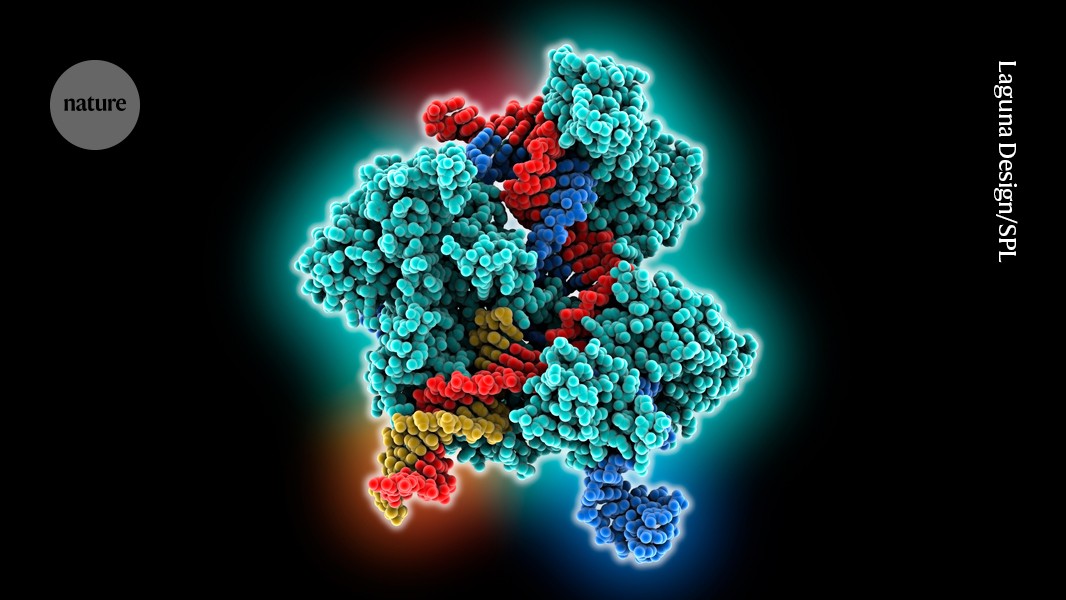
A genome-editing system more versatile than the classic CRISPR–Cas-9 complex (artist’s illustration) has been trialled in an 18-year-old with a genetic immune disorder.Credit: Laguna Design/Science Photo Library
The CRISPR family’s most versatile member has made its medical debut: a cutting-edge gene-editing technique known as prime editing has been used to treat a person for the first time. The recipient is a teenager with a rare immune disorder.
Researchers designed the treatment to correct some of the mutations that cause chronic granulomatous disease, a dangerous condition that disables a variety of immune cells, including those called neutrophils. A month after the teenager received the treatment, he had experienced no serious side effects. And the therapy seemed to have restored the function of a crucial enzyme in two-thirds of his neutrophils — more than enough to provide a significant boost to his immune system.
World’s first personalized CRISPR therapy given to baby with genetic disease
Prime Medicine, a biotechnology company in Cambridge, Massachusetts, unveiled the results on 19 May. It has not yet published them in a peer-reviewed journal.
It is too soon to know whether the treatment was a success: it will take between six months and a year to be certain that the edited stem cells are thriving, says Annarita Miccio, who studies gene therapy at the Imagine Institute at the Necker Hospital for Sick Children in Paris and is not involved in the research. But it is a promising approach to treating a difficult disease, she adds, and Prime Medicine’s previous results in mice1 were encouraging. “They put a lot of effort to design the perfect strategy that was very efficient in the long-term,” she says.
Investors needed
Despite these early signs of success, Prime Medicine also announced that it will not develop the therapy, called PM359, any further on its own. “Prime Medicine is exploring options for the continued clinical development of PM359 external to the company,” it said in a statement.
That decision reflects the harsh realities of developing gene-editing therapies for very rare diseases says David Liu, a chemical biologist at the Broad Institute of Harvard and MIT in Cambridge, Massachusetts, and a co-founder of Prime Medicine. “The science has moved far enough that many patients would benefit from these gene-editing treatments,” he says. “But it boils down to an issue not just of science and technology, but of economics.”
Upgrade your gene editor
The only gene-editing therapy currently on the market is a CRISPR–Cas9-based treatment for two blood disorders, sickle-cell disease and β-thalassaemia. This costs more than US$2 million per dose and has faced a slow roll-out in the United States and the United Kingdom.
Super-precise CRISPR tool enters US clinical trials for the first time
But an array of improved genome-editing methods promises many treatment options beyond classic CRISPR–Cas9. “It’s like upgrading your iPhone,” says Joseph Hacia, a medical geneticist at the Keck School of Medicine of the University of Southern California in Los Angeles. “There are new versions coming out all the time and the tools are constantly being refined.”