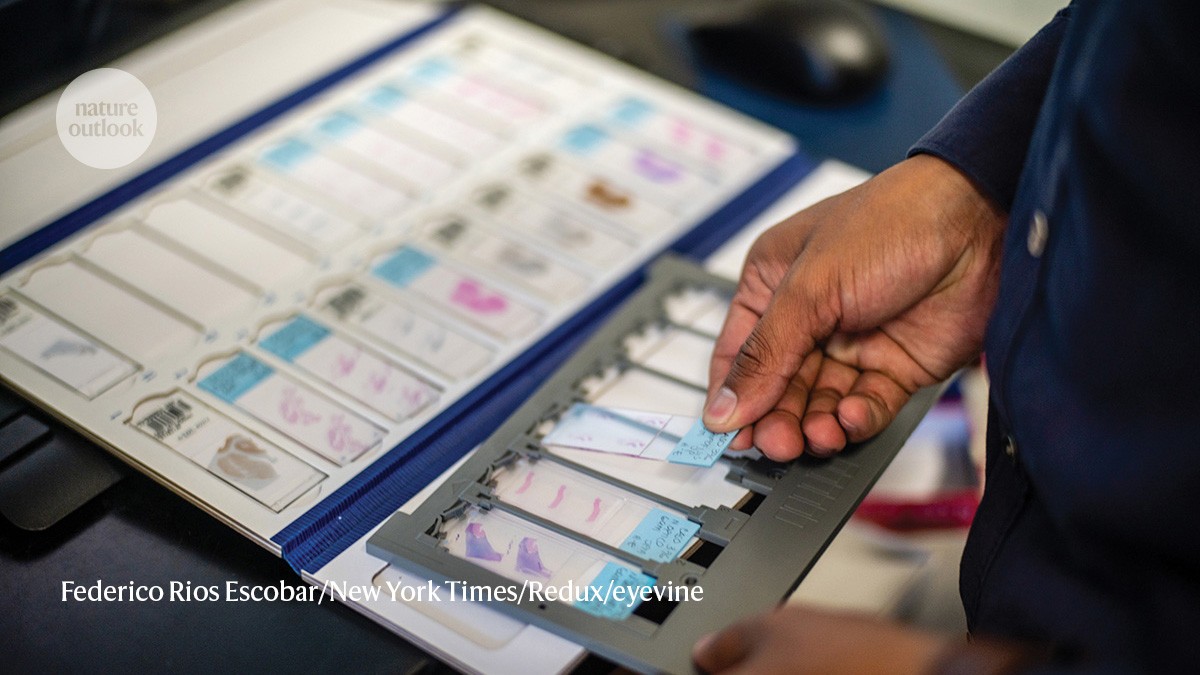
Brain-tissue slides in Medellín, Colombia.Credit: Federico Rios Escobar/New York Times/Redux/eyevine
In 1982, neurologist Francisco Lopera and his colleagues at the University of Antioquia in Medellín, Colombia, began studying a family for whom Alzheimer’s disease was a fact of life. Members of this family would invariably develop mild cognitive impairment at around 45 years of age. This would typically progress to dementia by the age of 50 as the hallmark protein plaques and tangles of Alzheimer’s accumulated in their brains, and death before their 60th birthday1.
Nature Outlook: Alzheimer’s disease
The early onset of the disease and its frequent occurrence in this extended family suggested a genetic cause. Lopera’s team, in collaboration with neuroscientist Kenneth Kosik, then at Harvard Medical School in Boston, Massachusetts, found that more than 100 affected people — all blood relatives — shared a mutation in the gene presenilin 1 (PSEN1)2. Mutations in presenilin genes are the most common cause of early-onset Alzheimer’s, and the Colombian cohort is the single largest group affected, with about 1,200 carriers of the mutation identified to this day.
But in every family, there is someone who goes against the grain. In this case, it is a person whose story challenges scientists’ understanding of Alzheimer’s disease pathology.
In 2019, researchers introduced the world to a woman born in rural Angostura, Colombia, who, like so many of her relatives, carried the PSEN1 mutation. But unlike them, she did not develop Alzheimer’s disease by the age of 50. Even at 72, she was barely showing symptoms. Her name was kept hidden until she died of cancer in 2020, one month shy of her 78th birthday. Today, researchers are still trying to work out why Aliria Rosa Piedrahita followed such a different path — and whether it might point the way to treatments that can help others.
A golden brain
Piedrahita used to joke that she had a “golden brain”, and a scan revealed what she might have meant. Her brain contained extremely high levels of amyloid-β plaques, but minimal neuroinflammation. Something else was missing, too. “The tangles of tau proteins that invariably accompany the plaques spared most of the brain — particularly those regions associated with clinical dementia,” says Kosik, now at the University of California, Santa Barbara. “Right away we learnt something important,” he says — that the plaques in her brain were not, in themselves, enough to cause cognitive issues.
Genetic testing showed that PSEN1 was not her only mutated gene. She also carried a mutated form of the gene APOE. One form of this gene, APOE4, is a major risk factor for late-onset Alzheimer’s disease. Two other versions are associated with either lower risk (APOE2) or typically have no effect (APOE3).
Piedrahita had two copies of the most common version, APOE3. However, hers was a rare variant called APOE3 Christchurch or APOE3Ch. This mutation affects how the APOE protein binds to a sugar–protein compound called HSPG, which helps tau to propagate through the brain. APOE3Ch showed the lowest affinity for HSPG of any form of the protein; APOE4 showed the highest3.
Animal studies recreated the unusual pattern of proteins seen in Piedrahita’s brain. When the APOE3Ch mutation was introduced into mice that would otherwise develop disease similar to Alzheimer’s, it protected against neurodegeneration. These mice had fewer, less widespread tau tangles, less damage to neurons, and less cognitive impairment4. Moreover, reduced binding of APOE3Ch to HSPG triggered degradation of tau by myeloid cells in the brain. “This may explain why tau seeding and spreading was less,” says David Holtzman, a neurologist and neuroscientist at Washington University School of Medicine in St. Louis, Missouri, and senior author of the study.
A team led by Yadong Huang, a neuroscientist at the Gladstone Institutes in San Francisco, California, explored whether APOE3Ch could also protect against late-onset Alzheimer’s in different model systems. It found that engineering the mutation into the APOE4 gene reduces the accumulation of tau, as well as the neuroinflammation and neurodegeneration that would otherwise be expected5. “It is really striking that the Christchurch mutation can lead to such broad protection,” says Huang.
Basis for treatment
The mechanisms behind the protective effects of APOE3Ch suggest that blocking the interaction between APOE and HSPG might help to treat Alzheimer’s disease.
More from Nature Outlooks
In 2023, Huang and Lopera were part of a team led by Joseph Arboleda-Velasquez, a cell biologist at Massachusetts Eye and Ear in Boston, that developed a Christchurch-mimetic antibody named 7C11. In mice, the antibody binds to ApoE4 and disrupts its interaction with HSPG, reducing tau pathology6. Arboleda-Velasquez has co-founded a company to continue development, and hopes to progress the potential therapy to clinical trials by 2027.
Huang and his group are also developing antibodies to block APOE–HSPG interaction, screening smaller molecules that could be easier to deliver to the brain, and exploring gene therapies. Holtzman is pursuing drugs inspired by the Christchurch mutation, with a focus on cells in the brain known as microglia.
Therapies inspired by Piedrahita’s brain have the potential to help not only the majority of people with late-onset Alzheimer’s, but also those whose genetics leave them at risk of early-onset disease. This includes thousands of people in Colombia with family ties to Piedrahita, brought into the research fold over many decades by Lopera’s efforts to build trust. Kosik expects that these people will continue to aid in the development of these drugs by taking part in future clinical trials. “It is remarkable that a treatment for Alzheimer’s disease could come directly from the remote villages in Colombia,” he says.