Once a week, early in the morning, community health worker Kiden Josephine Francis Laja mounts her bicycle and pedals as far as 10 miles away from her small village in South Sudan. Some weeks Laja is doing outreach, spending her day educating a community about which vaccines she can provide and what diseases they prevent. “It’s my responsibility to tell the mothers to bring the children for vaccination,” she says. She answers their questions and lets them know she’ll be back, usually the following week, to vaccinate their children. Late in the evening she mounts her bike and heads home.
When Laja returns with the vaccines, kept in a cooler with ice packs, she will spend the day immunizing anywhere from a few to 200 children against a range of diseases: polio, tetanus, diphtheria, pertussis, hepatitis B, influenza, bacterial meningitis, tuberculosis and, more recently, COVID. Most people in high-income countries haven’t seen these diseases in decades, but the people of South Sudan know them well. Many have seen family and friends die from them.
During the rest of the week Laja works at the community health center in her village of Pure, monitoring the solar-powered refrigerator and the vials inside. She vaccinates anyone who comes to the facility and metes out drugs for a few maladies such as ulcers, malaria and typhoid. But the village doesn’t have antibiotics—or electricity. Villagers grow their own food, raise goats and chickens, and get their water from wells in the ground.
Innovations In Solutions For Health Equity
It’s not easy work for just $102 a month, especially when it sometimes takes three months for the 25-year-old mother of two to get her pay. When it rains on travel days, she and her outreach pamphlets get soaked. She must regularly check the temperature of the vials in the cooler and replace the ice packs at just the right time to ensure the vaccines don’t go bad.
People in South Sudan don’t have much, but they have this program. “Vaccines are very important to me and my community and even to my country,” Laja says. During a large outbreak of measles that began in 2022 in the country, thousands of children suffered from the disease, and many died, leading to a nationwide vaccination campaign in 2023. “Now in our community you cannot find cases of measles,” she says.
Around the globe the measles vaccine has saved nearly 94 million lives over the past 50 years. This and other vaccinations have revolutionized global health. “Immunization is the most universal innovation that we have across humankind,” says Orin Levine, a fellow at the Center for Global Development in Washington, D.C. He notes that there are people around the world without access to telephones or even toilets, but they find ways to get their children immunized. “It’s the innovation that demonstrates what is possible in terms of delivery of service to everyone everywhere.”
A May study in the Lancet estimated that vaccines against 14 common pathogens have saved 154 million lives over the past five decades—at a rate of six lives every minute. They have cut infant mortality by 40 percent globally and by more than 50 percent in Africa. Throughout history vaccines have saved more lives than almost any other intervention. And vaccines’ promotion of health equity goes far beyond preventing death. The Lancet study found that each life saved through immunization resulted in an average 66 years of full health, without the long-term problems that many diseases cause. Vaccines play a role in nearly every measurement of health equity, from improving access to care, to reducing disability and long-term morbidity, to preventing loss of labor and the death of caretakers.
“We say vaccines are one of humanity’s great achievements in terms of having furthered the lifespan and life quality for humanity in the past 50 years,” says Aurélia Nguyen, chief program officer at Gavi, the Vaccine Alliance, a public-private partnership that works to ensure low- and middle-income countries have access to vaccines against more than 20 infectious diseases. Of all the different health interventions that exist, she says, “vaccines have the widest reach across the world.” The clearest evidence of vaccines’ impact on equity is that they are often the first intervention introduced into a community with no other health-care resources.
“When you don’t have a health worker or health system, there’s nothing. If you have no money, then you want the best bang for the buck, and it’s going to be immunization,” says Seth Berkley, former CEO of Gavi. “For every dollar you invest in immunization, you get $54 of benefit. From a cost-effectiveness point of view, it’s the best investment, so it tends to be the intervention that gets out to those communities first. And once you do that, you have a health worker who’s visiting those communities on a regular basis, and then that begins to start the conversation toward more primary health care, and that leads to getting a basic clinic set up. Immunization is the vanguard of the health system.”
Every country in the world has an immunization program thanks to the World Health Organization’s Expanded Program on Immunization, which was established in 1974. “Every single country and territory” has access to at least some vaccines, says Kate O’Brien, director of the WHO’s immunization, vaccines and biologicals department. Poverty, malnutrition, underlying health conditions, overcrowding, human conflict, displacement, and lack of access to medical care, hygiene or sanitation—all of these are risk factors for infectious disease, O’Brien says. Vaccines’ ability to reduce disease in the settings most plagued by these problems gives them disproportionate power to improve equity.
There may be no greater demonstration of vaccines’ power to deliver health equity than their success with smallpox. “The magnitude of the accomplishment of having eradicated smallpox, where absolutely nobody on this earth gets the disease,” O’Brien says, “that’s the ultimate in the issue of equity.”
A version of a smallpox vaccine was developed in 1796, and in 1959 global health experts decided to pursue full eradication. In the decade that followed, it became clear that such an ambitious goal would require more than political will. Although smallpox had been eliminated from North America and Europe, frequent outbreaks continued in South America, Africa and Asia.
In 1967 the WHO started its Intensified Eradication Program, which prompted a series of innovations. The bifurcated needle, which was developed around that time, allowed for smaller doses and required less user expertise for vaccine delivery than the previously favored jet injector. Researchers created a surveillance system to better track disease and vaccinate close contacts of infected people, making mass vaccination campaigns more effective. The last documented case of smallpox occurred in Somalia in 1977, and the WHO declared smallpox officially eradicated three years later.
That success inspired a similarly lofty goal in 1988 that has proved far more challenging: eradicating polio. Since the establishment of the Global Polio Eradication Initiative, cases have fallen 99 percent worldwide, but that last 1 percent is taking decades longer than planned. Public health experts now recognize that very few diseases can be completely eradicated through immunizations. Even so, they aim to decrease vaccine-preventable diseases to such low levels that severe morbidity and mortality are negligible. The WHO’s renamed Essential Program on Immunization initially focused on six childhood diseases: polio; measles; disseminated tuberculosis, the form of the disease most common in children; and diphtheria, tetanus and pertussis, for which children receive the combined DTP vaccine. It has now expanded to include vaccines against 13 diseases.
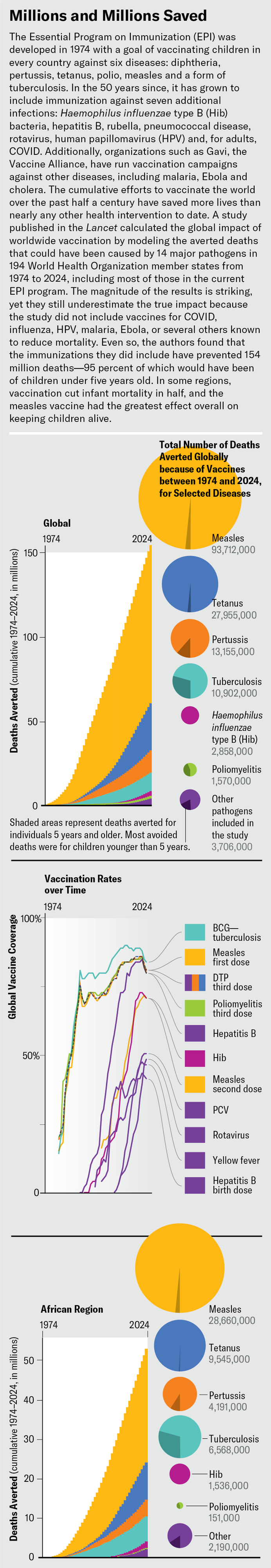
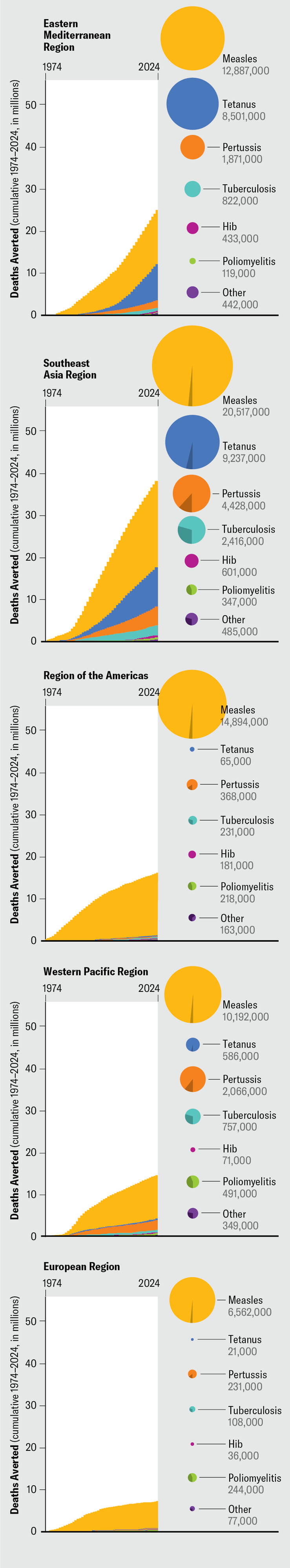
Source: Shattock, A. J. et al. Lancet 403, 2307–2316 (2024). Graphics styled by Jen Christiansen
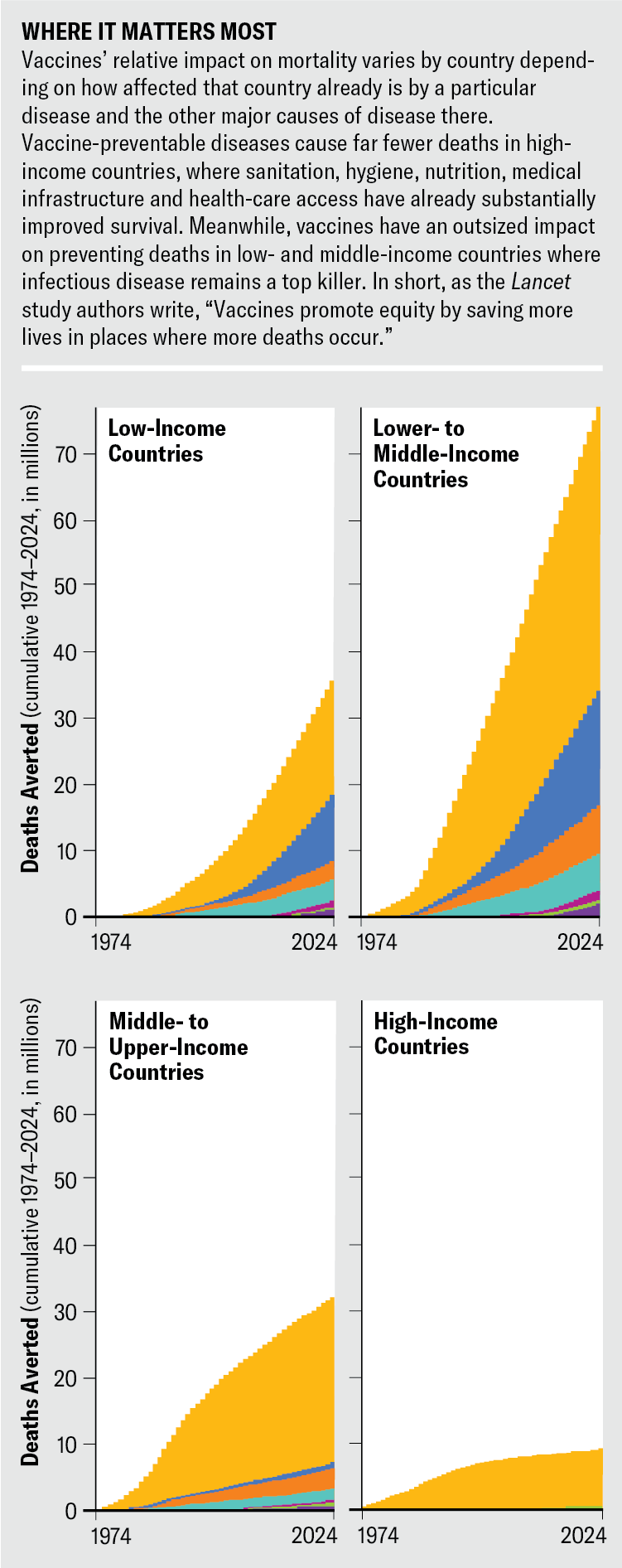
Source: Shattock, A. J. et al. Lancet 403, 2307–2316 (2024). Graphics styled by Jen Christiansen
“We have to look backward, in some ways, to realize how far we’ve really gone,” says Lois Privor-Dumm of Johns Hopkins University, who recently retired from her role as a senior research associate. “There has been tremendous progress over the past 50 years, and what is really left is making sure the equity agenda is really a focus.”
Now the question is how best to do it. A raft of technological and policy innovations aim to help. Before the WHO’s current vaccination program began, fewer than 5 percent of the world’s babies had access to routine immunizations. Today 84 percent of infants have received three doses of the DTP vaccine, the metric used to assess global immunization coverage.
“[Vaccines] level the playing field in terms of who gets these diseases and who doesn’t,” says Nicole Lurie, U.S. director of the Coalition for Epidemic Preparedness Innovations (CEPI), a foundation formed specifically to develop and improve access to vaccines for diseases that lack strong market demand. “But frankly, it was a really long road to get to that kind of equity.”
Setbacks through the 1990s led global health leaders to rethink their approach, and in 2000 Gavi was founded collaboratively by the WHO, UNICEF, the World Bank and the Gates Foundation. Thanks to Gavi, says Violaine Mitchell, director of immunization at the Gates Foundation, “now countries not only assume but demand that when a vaccine is introduced in the developed world, it’s also made available in the developing world.”
Gavi has vaccinated more than one billion children with a routine suite of shots and given a total of 1.8 billion immunizations to people of all ages through campaigns for illnesses such as measles in Ethiopia, Afghanistan and Somalia and yellow fever in Congo, averting more than 17 million deaths through 2022. Since Gavi was established, there has been a 70 percent reduction in deaths from vaccine-preventable diseases in children living in the lower-income countries the alliance supports, and mortality among children younger than five years in those countries has been halved. The pneumococcal and rotavirus vaccines have been particularly significant—pneumonia and diarrhea are among the top global killers of children under five.
But even those impressive numbers don’t fully capture the dramatic ways vaccines advance health equity. For example, epidemics of meningococcal meningitis were common in the “meningitis belt,” a stretch of 26 countries just south of the Sahara desert that has the highest rates of meningococcal disease in the world. Up to half of those infected die without treatment; even with treatment, one in 10 people dies. Since the development and distribution of a vaccine against meningitis A, this form of the disease has been nearly eliminated. The vaccine has not only saved lives but prevented long-term effects that meningitis survivors often suffer, including hearing loss, seizures, limb amputations or weakness, scarring, vision problems and cognitive difficulties.
Another example is the human papillomavirus (HPV) vaccine, which can prevent up to 90 percent of HPV-related cancers, including nearly all cervical cancer. Because high-income countries implemented cervical cancer screening programs decades ago, 94 percent of global deaths from cervical cancer in 2022 were in low- and middle-income countries. Gavi programs have vaccinated more than 16 million girls worldwide against HPV, and the organization aims to vaccinate 86 million by 2025. The physical benefits won’t be seen for years—it takes up to two decades for an HPV infection to develop into cancer—but the ripple effects of prevention go far beyond saving a single person’s life. A death from cervical cancer may mean loss of a family caretaker, loss of income and difficulty meeting children’s continuing health needs. “The tsunami effect of losing a mother to children, especially for those who are not economically stable, is devastating to a family,” O’Brien says. “Their lives are entirely dependent on the survival of that person.”
Vaccination can be a key entry point to additional health care. William Foege, a former director of the U.S. Centers for Disease Control and Prevention, who was instrumental in leading smallpox eradication and in setting up Gavi, called vaccines “the tugboat” for preventive care.
When health workers arrive to vaccinate children in a community, they can assess other children’s growth trajectories and nutritional issues, provide vitamin A supplements where there are deficiencies, distribute deworming tablets, monitor mosquito-borne diseases and check on additional needs. “If you manage to reach a child and give them a measles vaccine, then you may be able to give their mother maternal services,” Nguyen says. “It’s a perfect time to say: Are you sleeping under a bed net? Do you need a bed net? What are you doing for family planning?” Mitchell says. “All those conversations can come about because of the contact between the caregiver and the health worker that wouldn’t [otherwise] happen.”
In 1985 Rotary International launched its PolioPlus program, which used vaccination campaigns as an opening for other health interventions. “When Rotary and its partners added other things to improve the health systems of countries, it was a game changer,” says Stella Anyangwe, a Rotary International EndPolioNow coordinator and former WHO official. By strengthening laboratory systems, the cold-chain network of refrigerated storage necessary for transporting the vaccine, and overall disease surveillance, she says, improving systems for polio eradication “strengthened the health systems in general.” In short, Levine says, “immunization is an innovation that is pulling other innovations along.”
It can also free up valuable time and resources in health care. As infectious disease incidence falls, health workers and hospital beds become available for people with other conditions. This may already be happening with malaria. In Burkina Faso, about two out of every five visits to a health-care provider are for malaria, which historically accounts for more than 60 percent of the country’s hospitalizations. Similarly, malaria cases make up about half of hospitalizations in Cameroon; most of those patients are children under five who are eligible for the malaria vaccine. Although current malaria vaccines don’t prevent infection altogether, they reduce severe disease by 30 percent and all-cause mortality by 13 percent. Gavi began rolling out vaccination campaigns against malaria last year, providing 18 million doses to a dozen African countries, and malaria deaths have already begun falling. “You can imagine how much that’s going to free up capacity for health-care workers to focus on other [issues],” Nguyen says.
Vaccines help countries with fewer resources protect themselves from disease. Outbreaks disproportionately affect poorer areas: the 2014–2016 Ebola epidemic in West Africa, for example, devastated the region’s health-care infrastructure. Since the development of an Ebola vaccine in the late 2010s, subsequent outbreaks have remained comparatively small. And the current outbreak of mpox, which led the WHO to declare a global public health emergency in August, is being managed with vaccines that became available only in the past few years.
Gavi now supports stockpiles of outbreak-specific vaccines for cholera, yellow fever, meningococcal disease and Ebola so the countries most affected can focus their health-care resources on chronic disease, snakebites, cancer and HIV, among other conditions.
In late 2019, when a novel coronavirus detected in Wuhan, China, kicked off one of the largest, deadliest pandemics in a century, everyone looked to the same solution: a vaccine. COVID’s devastation hit poorer countries with less developed health-care systems particularly hard, and in wealthier countries people from underserved and low-income communities suffered higher rates of illness, death and economic hardship. It was clear that a COVID vaccine would be the most equitable solution.
The U.S. quickly directed $10 billion toward vaccine development, and dozens of other countries allocated what they could. The effort broke every record for the fastest vaccine development. The Chinese CDC released the sequence of SARS-CoV-2 on January 10, 2020, and just 11 months later, on December 8, 2020, the first COVID vaccine was administered outside of a clinical trial.
Officials at Gavi, UNICEF, WHO and CEPI quickly organized Covax, an international effort to accelerate COVID vaccine development and “to guarantee fair and equitable access for every country in the world,” according to the WHO. Covax delivered nearly two billion vaccines to more than 140 countries in the two years after the vaccines’ introduction, “by far the fastest, largest and most effective public health roll-out in history,” a Gavi spokesperson says. A 2022 study in the Lancet Infectious Diseases estimates that COVID vaccination worldwide prevented 19.8 million excess deaths, 7.4 million of those in Covax countries.
The challenges were steep and vaccine distribution contentious. “At no point did a richer country with access to vaccine doses choose to slow down its rollout to make doses available for people at higher risk in lower-income countries,” Levine says. “That’s vaccine nationalism, and it undermined the success of hardworking folks at Covax.”
Those problems have prompted a lot of reflection and a lot of new action. The organizations behind Covax have now set their sights on improving vaccine equity during future pandemics. Because Africa lacked vaccine access and had few manufacturing capabilities of its own, the new efforts are particularly focused on boosting the continent’s vaccine-manufacturing capabilities. The Africa CDC has partnered with other organizations to create the Partnerships for African Vaccine Manufacturing with a goal of making 60 percent of its needed vaccines by 2040. In June 2024 Gavi launched the African Vaccine Manufacturing Accelerator, a financing program developed with the Africa CDC and African Union to put up to $1.2 billion over the next decade toward building up the continent’s vaccine-manufacturing capacity.
In the almost 25 years since Gavi was launched, it has made substantial progress in advancing equity in vaccine manufacturing. In 2000 four of its five vaccine suppliers were in wealthy countries. Today most of its 20 or so suppliers are in developing countries. “It opened up a marketplace for large-scale, low-cost manufacturing in India, in Brazil, in China and in Indonesia,” says Berkley, former Gavi CEO.
It will still be immensely challenging to get vaccines into the arms and mouths of people who need them most. Health workers must find and immunize zero-dose children—children who have yet to receive vaccines of any kind, like the ones Laja sees in South Sudan. And low-income countries must acquire the financing and build the infrastructure to facilitate that process. Then Laja and her peers must educate people so fear does not become a barrier to access.
Workers such as Laja are part of the global workforce that the WHO, Gavi, UNICEF, the Gates Foundation, Rotary, and other organizations have trained to use vaccines against disease and health disparities. Earlier this year Laja completed training in preparation for South Sudan’s malaria-vaccine rollout. In 2022 there were almost 7,000 malaria deaths in South Sudan, and the disease is the top killer of young children in the country. The previous year South Sudan’s malaria fatalities accounted for more than 1.2 percent of the total worldwide.
Laja is eager to see the vaccines’ impact on her community and in the villages she visits, where parents will walk for miles from outlying areas to meet her. “There are very few things women and caretakers will walk hours and hours for, but vaccines are still one of them,” says Mitchell of the Gates Foundation. “People will literally drop everything to come and vaccinate their child.”