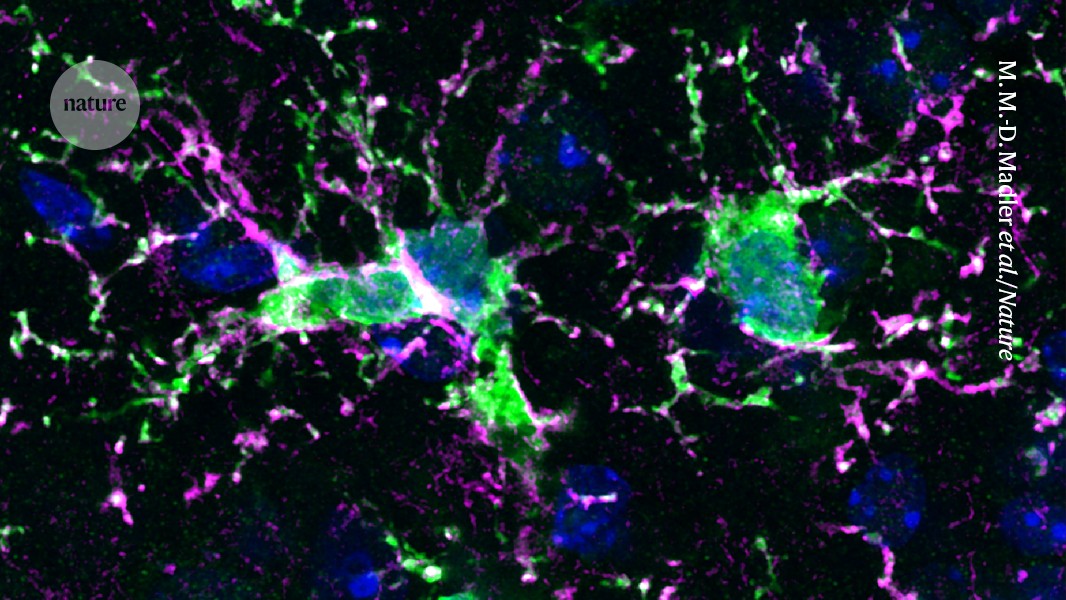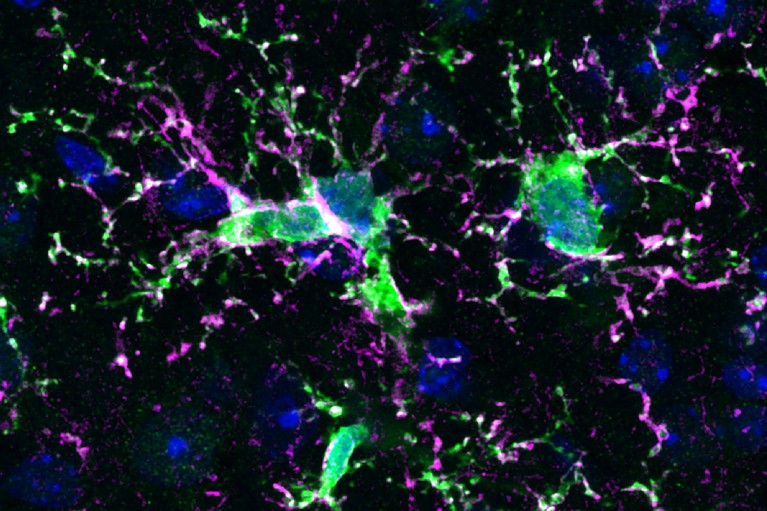
After a mouse received treatment to eliminate immune cells called microglia, it was injected with human progenitor cells that developed into human immune cells (green, pink and blue) in the animal’s brain.Credit: M. M.-D. Madler et al./Nature
A fresh supply of the immune cells that keep the brain tidy might one day help to treat a host of conditions, from ultra-rare genetic disorders to more familiar scourges, such as Alzheimer’s disease.
In the past few months, a spate of new studies have highlighted the potential of a technique called microglia replacement and explored ways to make it safer and more effective. “This approach is very promising,” says Pasqualina Colella, who studies gene and cell therapy at Stanford University School of Medicine in California. “But the caveat is the toxicity of the procedure.”
New hope for Alzheimer’s: lithium supplement reverses memory loss in mice
Microglia are immune cells that patrol the brain, gobbling up foreign invaders, damaged cells and harmful substances. They can help to protect neurons — cells that transmit and receive messages to and from other tissues — during seizures and strokes, and they prune unneeded connections between neurons during normal brain development.
“Microglia do a lot of important things,” says Chris Bennett, a psychiatrist who studies microglia at the Children’s Hospital of Philadelphia in Pennsylvania. “So, it’s not surprising that they are involved in the pathogenesis of many diseases.”
Those diseases include a suite of rare disorders caused by genetic mutations that directly affect microglia. Malfunctioning microglia have also been implicated in more familiar conditions with complex causes, such as Alzheimer’s disease and Parkinson’s disease, as well as ageing, says Bo Peng, a neuroscientist at Fudan University in Shanghai, China.
Immune-cell swap
This has led researchers to investigate a tantalizing possibility: that replacing disease-causing microglia could treat some brain conditions. But swapping out microglia poses special challenges. Physicians typically replace a person’s immune cells by performing a bone-marrow transplant, which provides a fresh supply of stem cells that shelter in the bone marrow and give rise to many immune cells. Microglia, however, reside almost exclusively in the central nervous system, and typically replenish themselves by division rather than relying on stem cells in the bone marrow to send in replacements.
How CRISPR gene editing could help treat Alzheimer’s
Physicians already use bone-marrow transplants to treat some rare diseases that affect microglia, such as a condition called X-linked adrenoleukodystrophy. The treatment can be effective, says Marco Prinz, a neuropathologist at the University of Freiburg in Germany, but the results are inconsistent and typically replace only a small percentage of the recipient’s natural microglia.
In July, Peng’s team used bone-marrow transplants to replace abnormal microglia resulting from a fatal brain disease called CAMP (CSF1R-associated microgliopathy). The treatment was a success in both mice and in a small trial of eight people with the rare disorder: none of the eight participants experienced a decline in their motor or cognitive abilities in two years following the treatment1, whereas members of a control group who did not receive the procedure experienced a deterioration of both.
One possible reason for the success of the CAMP trial is the nature of the disease itself, says Bennett, because people with CAMP tend to produce relatively few microglia. This could leave space for the transplanted cells to thrive.
Onerous regimen
Creating that niche for the new microglia is a pivotal step in microglia replacement — and a source of concern. To make room for transplanted cells, physicians must first wipe out as many of the brain’s resident microglia as possible. This can entail high levels of chemotherapy or radiotherapy, both of which can leave the recipient vulnerable to infection during the procedure and raise their long-term risk of cancer. That means that microglia replacement is, for the moment, too toxic to be used except in severe, rapidly progressing diseases such as CAMP, says Colella.