Global Tuberculosis Report 2023 (World Health Organization, 2023); www.who.int/teams/global-programme-on-tuberculosis-and-lung-health/tb-reports/global-tuberculosis-report-2023.
Dong, J., Krasnova, L., Finn, M. G. & Sharpless, K. B. Sulfur(VI) fluoride exchange (SuFEx): another good reaction for click chemistry. Angew. Chem. Int. Ed. 53, 9430–9448 (2014).
The Lancet Infectious Diseases. Tuberculosis at the United Nations: a missed chance. Lancet Infect. Dis. 18, 1161 (2018).
Gumbo, T. et al. Isoniazid’s bactericidal activity ceases because of the emergence of resistance, not depletion of Mycobacterium tuberculosis in the log phase of growth. J. Infect. Dis. 195, 194–201 (2007).
Neres, J. et al. Structural basis for benzothiazinone-mediated killing of Mycobacterium tuberculosis. Sci. Transl. Med. 4, 150ra121 (2012).
Hillebrand, L., Liang, X. J., Serafim, R. A. M. & Gehringer, M. Emerging and re-emerging warheads for targeted covalent inhibitors: an update. J. Med. Chem. 67, 7668–7758 (2024).
Rozwarski, D. A., Grant, G. A., Barton, D. H., Jacobs, W. R. & Sacchettini, J. C. Modification of the NADH of the isoniazid target (InhA) from Mycobacterium tuberculosis. Science 279, 98–102 (1998).
Barrow, A. S. et al. The growing applications of SuFEx click chemistry. Chem. Soc. Rev. 48, 4731–4758 (2019).
Gu, C. et al. Chemical proteomics with sulfonyl fluoride probes reveals selective labeling of functional tyrosines in glutathione transferases. Chem. Biol. 20, 541–548 (2013).
Gilbert, K. E. et al. Profiling sulfur(VI) fluorides as reactive functionalities for chemical biology tools and expansion of the ligandable proteome. ACS Chem. Biol. 18, 285–295 (2023).
Moss, D. E. et al. A randomized phase I study of methanesulfonyl fluoride, an irreversible cholinesterase inhibitor, for the treatment of Alzheimer’s disease. Br. J. Clin. Pharmacol. 75, 1231–1239 (2013).
Chen, W. et al. Arylfluorosulfates inactivate intracellular lipid binding protein(s) through chemoselective SuFEx reaction with a binding site Tyr residue. J. Am. Chem. Soc. 138, 7353–7364 (2016).
Zhang, J. et al. Identification of simple arylfluorosulfates as potent agents against resistant bacteria. Proc. Natl Acad. Sci. USA 118, e2103513118 (2021).
Mukherjee, H. et al. A study of the reactivity of S(VI)-F containing warheads with nucleophilic amino-acid side chains under physiological conditions. Org. Biomol. Chem. 15, 9685–9695 (2017).
Baggio, C. et al. Aryl-fluorosulfate-based lysine covalent pan-inhibitors of apoptosis protein (IAP) antagonists with cellular efficacy. J. Med. Chem. 62, 9188–9200 (2019).
Martín-Gago, P. & Olsen, C. A. Arylfluorosulfate-based electrophiles for covalent protein labeling: a new addition to the arsenal. Angew. Chem. Int. Ed. Engl. 58, 957–966 (2019).
Huang, H. & Jones, L. H. Covalent drug discovery using sulfur(VI) fluoride exchange warheads. Expert Opin. Drug Discov. 18, 725–735 (2023).
Bolding, J. E. et al. Aryl fluorosulfate based inhibitors that covalently target the SIRT5 lysine deacylase. Angew. Chem. Int. Ed. Engl. 61, e202204565 (2022).
Alboreggia, G. et al. Covalent targeting of histidine residues with aryl fluorosulfates: application to Mcl-1 BH3 mimetics. J. Med. Chem. 67, 20214–20223 (2024).
Fadeyi, O. O. et al. Covalent enzyme inhibition through fluorosulfate modification of a noncatalytic serine residue. ACS Chem. Biol. 12, 2015–2020 (2017).
Gambini, L. et al. Covalent inhibitors of protein-protein interactions targeting lysine, tyrosine, or histidine residues. J. Med. Chem. 62, 5616–5627 (2019).
Gavalda, S. et al. The Pks13/FadD32 crosstalk for the biosynthesis of mycolic acids in Mycobacterium tuberculosis. J. Biol. Chem. 284, 19255–19264 (2009).
Wilson, R. et al. Antituberculosis thiophenes define a requirement for Pks13 in mycolic acid biosynthesis. Nat. Chem. Biol. 9, 499–506 (2013).
Aggarwal, A. et al. Development of a novel lead that targets M. tuberculosis polyketide synthase 13. Cell 170, 249–259 (2017).
Gavalda, S. et al. The polyketide synthase Pks13 catalyzes a novel mechanism of lipid transfer in mycobacteria. Chem. Biol. 21, 1660–1669 (2014).
Kim, S. K. et al. Structure and dynamics of the essential endogenous mycobacterial polyketide synthase Pks13. Nat. Struct. Mol. Biol. 30, 296–308 (2023).
Zhang, W. et al. Structure-based optimization of coumestan derivatives as polyketide synthase 13-thioesterase(Pks13-TE) inhibitors with improved hERG profiles for Mycobacterium tuberculosis treatment. J. Med. Chem. 65, 13240–13252 (2022).
Lun, S. et al. Therapeutic potential of coumestan Pks13 inhibitors for tuberculosis. Antimicrob. Agents Chemother. 95, e02190–20 (2023).
Wilson, C. et al. Optimization of TAM16, a benzofuran that inhibits the thioesterase activity of Pks13; evaluation toward a preclinical candidate for a novel antituberculosis clinical target. J. Med. Chem. 65, 409–423 (2022).
Krieger, I. V. et al. Inhibitors of the thioesterase activity of Mycobacterium tuberculosis Pks13 discovered using DNA-encoded chemical library screening. ACS Infect. Dis. 10, 1561–1575 (2024).
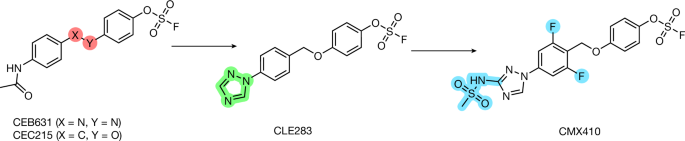
Yang, B. et al. Synthesis and structure–activity relationships of aryl fluorosulfate-based inhibitors as novel antitubercular agents. Bioorg. Med. Chem. Lett. 98, 129596 (2024).
Cook, G. M., Greening, C., Hards, K. & Berney, M. in Advances in Microbial Physiology Vol. 65 (ed. Poole, R. K.) 1–62 (Elsevier, 2014).
Hu, Y., Coates, A. R. & Mitchison, D. A. Sterilising action of pyrazinamide in models of dormant and rifampicin-tolerant Mycobacterium tuberculosis. Int. J. Tuberc. Lung Dis. 10, 317–322 (2006).
Hariguchi, N. et al. OPC-167832, a novel carbostyril derivative with potent antituberculosis activity as a DprE1 inhibitor. Antimicrob. Agents Chemother. 64, e02020–19 (2020).
Bergeret, F. et al. Biochemical and structural study of the atypical acyltransferase domain from the mycobacterial polyketide synthase Pks13. J. Biol. Chem. 287, 33675–33690 (2012).
Conradie, F. et al. Bedaquiline-pretomanid-linezolid regimens for drug-resistant tuberculosis. N. Engl. J. Med. 387, 810–823 (2022).
Lenaerts, A. J. et al. Preclinical testing of the nitroimidazopyran PA-824 for activity against Mycobacterium tuberculosis in a series of in vitro and in vivo models. Antimicrob. Agents Chemother. 49, 2294–2301 (2005).
Rosenthal, I. M. et al. Dose-ranging comparison of rifampin and rifapentine in two pathologically distinct murine models of tuberculosis. Antimicrob. Agents Chemother. 56, 4331–4340 (2012).
Li, S.-Y. et al. Bactericidal and sterilizing activity of a novel regimen with bedaquiline, pretomanid, moxifloxacin, and pyrazinamide in a murine model of tuberculosis. Antimicrob. Agents Chemother. 61, e00913–e00917 (2017).
Yamamoto, K., Nakata, N., Mukai, T., Kawagishi, I. & Ato, M. Coexpression of MmpS5 and MmpL5 contributes to both efflux transporter MmpL5 trimerization and drug resistance in Mycobacterium tuberculosis. mSphere 6, e00518–e00520 (2021).
Cho, S., Lee, H. S. & Franzblau, S. G. in Mycobacteria Protocols (eds Parish, T. et al.) 281–292 (Springer, 2015).
Pankey, G. A. & Sabath, L. D. Clinical relevance of bacteriostatic versus bactericidal mechanisms of action in the treatment of gram‐positive bacterial infections. Clin. Infect. Dis. 38, 864–870 (2004).
Lechartier, B., Hartkoorn, R. C. & Cole, S. T. In vitro combination studies of benzothiazinone lead compound BTZ043 against Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 56, 5790–5793 (2012).
Hall, M. J., Middleton, R. F. & Westmacott, D. The fractional inhibitory concentration (FIC) index as a measure of synergy. J. Antimicrob. Chemother. 11, 427–433 (1983).
Larsen, M. H., Biermann, K., Tandberg, S., Hsu, T. & Jacobs, W. R. Genetic manipulation of Mycobacterium tuberculosis. Curr. Protoc. Microbiol. 6, 10A.2.1–10A.2.21 (2007).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows–Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Eschenfeldt, W. H., Lucy, S., Millard, C. S., Joachimiak, A. & Mark, I. D. in High Throughput Protein Expression and Purification Vol. 498 (ed. Doyle, S. A.) 105–115 (Humana, 2009).
Otwinowski, Z. & Minor, W. in Methods in Enzymology Vol. 276 (eds Abelson, J. N. et al.) 307–326 (Elsevier, 1997).
Winn, M. D. et al. Overview of the CCP 4 suite and current developments. Acta Crystallogr. D 67, 235–242 (2011).
Liebschner, D. et al. Macromolecular structure determination using X-rays, neutrons and electrons: recent developments in. Phenix. Acta Crystallogr. Sect. Struct. Biol. 75, 861–877 (2019).
Emsley, P., Lohkamp, B., Scott, W. G. & Cowtan, K. Features and development of Coot. Acta Crystallogr. D 66, 486–501 (2010).
Pettersen, E. F. et al. UCSF Chimera—a visualization system for exploratory research and analysis. J. Comput. Chem. 25, 1605–1612 (2004).
Abagyan, R., Totrov, M. & Kuznetsov, D. ICM—a new method for protein modeling and design: applications to docking and structure prediction from the distorted native conformation. J. Comput. Chem. 15, 488–506 (1994).
Cho, S. H. et al. Low-oxygen-recovery assay for high-throughput screening of compounds against nonreplicating Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 51, 1380–1385 (2007).
Roberts, A. D. et al. in Methods in Microbiology (eds Kaufmann, S. & Kabelitz, D.) 433–462 (Academic, 2002).