Chiang, J. Y. Bile acid metabolism and signaling. Compr. Physiol. 3, 1191–1212 (2013).
de Aguiar Vallim, T. Q., Tarling, E. J. & Edwards, P. A. Pleiotropic roles of bile acids in metabolism. Cell Metab. 17, 657–669 (2013).
Wang, W., Seward, D. J., Li, L., Boyer, J. L. & Ballatori, N. Expression cloning of two genes that together mediate organic solute and steroid transport in the liver of a marine vertebrate. Proc. Natl Acad. Sci. USA 98, 9431–9436 (2001).
Seward, D. J., Koh, A. S., Boyer, J. L. & Ballatori, N. Functional complementation between a novel mammalian polygenic transport complex and an evolutionarily ancient organic solute transporter, OSTα–OSTβ. J. Biol. Chem. 278, 27473–27482 (2003).
Ballatori, N., Christian, W. V., Wheeler, S. G. & Hammond, C. L. The heteromeric organic solute transporter, OSTα-OSTβ/SLC51: a transporter for steroid-derived molecules. Mol. Aspects Med. 34, 683–692 (2013).
Dawson, P. A., Hubbert, M. L. & Rao, A. Getting the mOST from OST: role of organic solute transporter, OSTα-OSTβ, in bile acid and steroid metabolism. Biochim. Biophys. Acta 1801, 994–1004 (2010).
Gao, E. et al. Organic solute transporter α deficiency: a disorder with cholestasis, liver fibrosis, and congenital diarrhea. Hepatology 71, 1879–1882 (2020).
Sultan, M. et al. Organic solute transporter-β (SLC51B) deficiency in two brothers with congenital diarrhea and features of cholestasis. Hepatology 68, 590–598 (2018).
Ballatori, N. et al. OST α-OST β: a key membrane transporter of bile acids and conjugated steroids. Front. Biosci. 14, 2829–2844 (2009).
Beaudoin, J. J., Brouwer, K. L. R. & Malinen, M. M. Novel insights into the organic solute transporter α/β, OSTα/β: from the bench to the bedside. Pharmacol. Ther. 211, 107542 (2020).
Dawson, P. A., Lan, T. & Rao, A. Bile acid transporters. J. Lipid Res. 50, 2340–2357 (2009).
Ghallab, A. et al. Enteronephrohepatic circulation of bile acids and therapeutic potential of systemic bile acid transporter inhibitors. J. Hepatol. 83, 1204–1217 (2025).
Chiang, J. Y. Bile acids: regulation of synthesis. J. Lipid Res. 50, 1955–1966 (2009).
Ballatori, N. et al. OSTα-OSTβ: a major basolateral bile acid and steroid transporter in human intestinal, renal, and biliary epithelia. Hepatology 42, 1270–1279 (2005).
Dawson, P. A. et al. The heteromeric organic solute transporter α–β, Ostα–Ostβ, is an ileal basolateral bile acid transporter. J. Biol. Chem. 280, 6960–6968 (2005).
Ballatori, N., Fang, F., Christian, W. V., Li, N. & Hammond, C. L. Ostα–Ostβ is required for bile acid and conjugated steroid disposition in the intestine, kidney, and liver. Am. J. Physiol. Gastrointest. Liver Physiol. 295, G179–G186 (2008).
Ferrebee, C. B. et al. Organic solute transporter α–β protects ileal enterocytes from bile acid-induced injury. Cell. Mol. Gastroenterol. Hepatol. 5, 499–522 (2018).
Boyer, J. L. et al. Upregulation of a basolateral FXR-dependent bile acid efflux transporter OSTα–OSTβ in cholestasis in humans and rodents. Am. J. Physiol. Gastrointest. Liver Physiol. 290, G1124–G1130 (2006).
Malinen, M. M., Ali, I., Bezencon, J., Beaudoin, J. J. & Brouwer, K. L. R. Organic solute transporter OSTα/β is overexpressed in nonalcoholic steatohepatitis and modulated by drugs associated with liver injury. Am. J. Physiol. Gastrointest. Liver Physiol. 314, G597–G609 (2018).
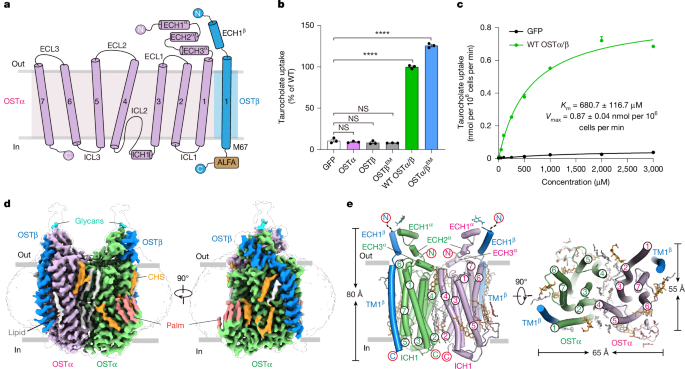
Christian, W. V., Li, N., Hinkle, P. M. & Ballatori, N. β-Subunit of the Ostα–Ostβ organic solute transporter is required not only for heterodimerization and trafficking but also for function. J. Biol. Chem. 287, 21233–21243 (2012).
Fang, F. et al. Neurosteroid transport by the organic solute transporter OSTα–OSTβ. J. Neurochem. 115, 220–233 (2010).
Suga, T., Yamaguchi, H., Ogura, J. & Mano, N. Characterization of conjugated and unconjugated bile acid transport via human organic solute transporter α/β. Biochim. Biophys. Acta Biomembr. 1861, 1023–1029 (2019).
Li, J. et al. The role of a basolateral transporter in rosuvastatin transport and its interplay with apical breast cancer resistance protein in polarized cell monolayer systems. Drug Metab. Dispos. 40, 2102–2108 (2012).
Li, N., Cui, Z., Fang, F., Lee, J. Y. & Ballatori, N. Heterodimerization, trafficking and membrane topology of the two proteins, Ostα and Ostβ, that constitute the organic solute and steroid transporter. Biochem. J. 407, 363–372 (2007).
Gotzke, H. et al. The ALFA-tag is a highly versatile tool for nanobody-based bioscience applications. Nat. Commun. 10, 4403 (2019).
Jumper, J. et al. Highly accurate protein structure prediction with AlphaFold. Nature 596, 583–589 (2021).
Christian, W. V. & Hinkle, P. M. Global functions of extracellular, transmembrane and cytoplasmic domains of organic solute transporter β-subunit. Biochem. J. 474, 1981–1992 (2017).
Chatzikyriakidou, Y., Ahn, D. H., Nji, E. & Drew, D. The GFP thermal shift assay for screening ligand and lipid interactions to solute carrier transporters. Nat. Protoc. 16, 5357–5376 (2021).
Soroka, C. J., Xu, S., Mennone, A., Lam, P. & Boyer, J. L. N-glycosylation of the α subunit does not influence trafficking or functional activity of the human organic solute transporter α/β. BMC Cell Biol. 9, 57 (2008).
Shaye, H. et al. Structural basis of the activation of a metabotropic GABA receptor. Nature 584, 298–303 (2020).
Josephs, T. M. et al. Structure and dynamics of the CGRP receptor in apo and peptide-bound forms. Science 372, eabf7258 (2021).
Goutam, K., Ielasi, F. S., Pardon, E., Steyaert, J. & Reyes, N. Structural basis of sodium-dependent bile salt uptake into the liver. Nature 606, 1015–1020 (2022).
Shan, Z. et al. Cryo-EM structures of human organic anion transporting polypeptide OATP1B1. Cell Res. 33, 940–951 (2023).
Liu, H. et al. Structural basis of bile salt extrusion and small-molecule inhibition in human BSEP. Nat. Commun. 14, 7296 (2023).
Xu, S. et al. A novel di-leucine motif at the N-terminus of human organic solute transporter β is essential for protein association and membrane localization. PLoS One 11, e0158269 (2016).
Lu, Y. et al. Characterization of a novel organic solute transporter homologue from Clonorchis sinensis. PLoS Negl. Trop. Dis. 12, e0006459 (2018).
Taghon, G. J., Rowe, J. B., Kapolka, N. J. & Isom, D. G. Predictable cholesterol binding sites in GPCRs lack consensus motifs. Structure 29, 499–506 (2021).
Malinen, M. M. et al. Novel in vitro method reveals drugs that inhibit organic solute transporter α/β (OSTα/β). Mol. Pharm. 16, 238–246 (2019).
Hu, N. J., Iwata, S., Cameron, A. D. & Drew, D. Crystal structure of a bacterial homologue of the bile acid sodium symporter ASBT. Nature 478, 408–411 (2011).
Ji, J. et al. Plant SWEET family of sugar transporters: structure, evolution and biological functions. Biomolecules 12, 205 (2022).
Naes, S. M., Ab-Rahim, S., Mazlan, M. & Abdul Rahman, A. Equilibrative nucleoside transporter 2: properties and physiological roles. Biomed Res. Int. 2020, 5197626 (2020).
Latorraca, N. R. et al. Mechanism of substrate translocation in an alternating access transporter. Cell 169, 96–107 (2017).
Wright, N. J. & Lee, S. Y. Structures of human ENT1 in complex with adenosine reuptake inhibitors. Nat. Struct. Mol. Biol. 26, 599–606 (2019).
Marin, J. J., Macias, R. I., Briz, O., Banales, J. M. & Monte, M. J. Bile acids in physiology, pathology and pharmacology. Curr. Drug Metab. 17, 4–29 (2015).
Ticho, A. L. et al. S-acylation modulates the function of the apical sodium-dependent bile acid transporter in human cells. J. Biol. Chem. 295, 4488–4497 (2020).
Ayewoh, E. N., Czuba, L. C., Nguyen, T. T. & Swaan, P. W. S-acylation status of bile acid transporter hASBT regulates its function, metabolic stability, membrane expression, and phosphorylation state. Biochim. Biophys. Acta Biomembr. 1863, 183510 (2021).
Khelashvili, G. & Menon, A. K. Phospholipid scrambling by G protein-coupled receptors. Annu. Rev. Biophys. 51, 39–61 (2022).
Frankenberg, T. et al. Regulation of the mouse organic solute transporter α–β, Ostα–Ostβ, by bile acids. Am. J. Physiol. Gastrointest. Liver Physiol. 290, G912–G922 (2006).
Rao, A. et al. The organic solute transporter α–β, Ostα–Ostβ, is essential for intestinal bile acid transport and homeostasis. Proc. Natl Acad. Sci. USA 105, 3891–3896 (2008).
Sakuragi, T. & Nagata, S. Regulation of phospholipid distribution in the lipid bilayer by flippases and scramblases. Nat. Rev. Mol. Cell Biol. 24, 576–596 (2023).
Kalienkova, V. et al. Stepwise activation mechanism of the scramblase nhTMEM16 revealed by cryo-EM. eLife 8, e44364 (2019).
Xia, Z. et al. Structural insights into glucose-6-phosphate recognition and hydrolysis by human G6PC1. Proc. Natl Acad. Sci. USA 122, e2418316122 (2025).
Wu, D. et al. Transport and inhibition mechanisms of human VMAT2. Nature 626, 427–434 (2024).
Zivanov, J. et al. New tools for automated high-resolution cryo-EM structure determination in RELION-3. eLife 7, e42166 (2018).
Zheng, S. Q. et al. MotionCor2: anisotropic correction of beam-induced motion for improved cryo-electron microscopy. Nat. Methods 14, 331–332 (2017).
Zhang, K. Gctf: real-time CTF determination and correction. J. Struct. Biol. 193, 1–12 (2016).
Punjani, A., Rubinstein, J. L., Fleet, D. J. & Brubaker, M. A. cryoSPARC: algorithms for rapid unsupervised cryo-EM structure determination. Nat. Methods 14, 290–296 (2017).
Pettersen, E. F. et al. UCSF Chimera—a visualization system for exploratory research and analysis. J. Comput. Chem. 25, 1605–1612 (2004).
Emsley, P. & Cowtan, K. Coot: model-building tools for molecular graphics. Acta Crystallogr. D 60, 2126–2132 (2004).
Afonine, P. V. et al. Real-space refinement in PHENIX for cryo-EM and crystallography. Acta Crystallogr. D 74, 531–544 (2018).
Pettersen, E. F. et al. UCSF ChimeraX: structure visualization for researchers, educators, and developers. Protein Sci. 30, 70–82 (2021).
Jo, S., Kim, T., Iyer, V. G. & Im, W. CHARMM-GUI: a web-based graphical user interface for CHARMM. J. Comput. Chem. 29, 1859–1865 (2008).
Maier, J. A. et al. ff14SB: improving the accuracy of protein side chain and backbone parameters from ff99SB. J. Chem. Theory Comput. 11, 3696–3713 (2015).
Dickson, C. J., Walker, R. C. & Gould, I. R. Lipid21: complex lipid membrane simulations with AMBER. J. Chem. Theory Comput. 18, 1726–1736 (2022).
Wang, J., Wang, W., Kollman, P. A. & Case, D. A. Automatic atom type and bond type perception in molecular mechanical calculations. J. Mol. Graph. Model. 25, 247–260 (2006).
Jakalian, A., Jack, D. B. & Bayly, C. I. Fast, efficient generation of high-quality atomic charges. AM1-BCC model: II. Parameterization and validation. J. Comput. Chem. 23, 1623–1641 (2002).
Sousa da Silva, A. W. & Vranken, W. F. ACPYPE—AnteChamber PYthon Parser interfacE. BMC Res. Notes 5, 367 (2012).
Barducci, A., Bussi, G. & Parrinello, M. Well-tempered metadynamics: a smoothly converging and tunable free-energy method. Phys. Rev. Lett. 100, 020603 (2008).
Hess, B., Kutzner, C., van der Spoel, D. & Lindahl, E. GROMACS 4: algorithms for highly efficient, load-balanced, and scalable molecular simulation. J. Chem. Theory Comput. 4, 435–447 (2008).
Beránek, J., Křenek, A. & Spiwok, V. Analysis of metadynamics simulations by metadynminer.py. Bioinformatics 40, btae614 (2024).
Gonzalez-Aleman, R., Hernandez-Castillo, D., Caballero, J. & Montero-Cabrera, L. A. Quality threshold clustering of molecular dynamics: a word of caution. J. Chem. Inf. Model. 60, 467–472 (2020).