Cognitive tests would be used less often to diagnose Alzheimer’s disease under a proposal by some scientists.Credit: Burger/Phanie/Science Photo Library
Controversy has erupted among researchers over an effort to adopt blood tests and brain scans for diagnosing Alzheimer’s disease, rather than the cognitive screening that has been used for decades.
Proponents of the change say that new biomarker tests can detect Alzheimer’s at a very early stage — the best time to apply any treatments that are developed to reverse the disease. But critics say that, although the effort is well-intentioned, it means that people can be diagnosed with a single test, even if they have no symptoms of cognitive decline — and might never develop them.
“There’s a risk of misunderstanding and distress that individuals who are asymptomatic will have if we tell them they have Alzheimer’s, whereas nothing will happen in their lifetime in a majority of cases,” says Nicolas Villain, a neurologist at Sorbonne University in Paris, who co-wrote a paper1 published on 1 November in JAMA Neurology criticizing the new diagnostic criteria.
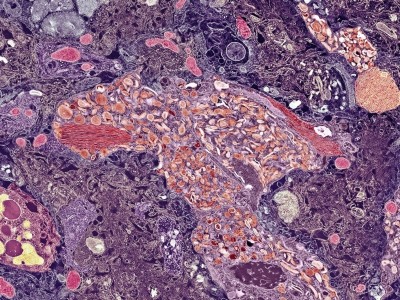
Plaques and tangles
The brains of people with Alzheimer’s have two key features: plaques of sticky amyloid-β proteins and tangles formed from tau proteins. The neurodegeneration linked with the development of these plaques and tangles is irreversible, so researchers have been searching for treatments to give to healthy people to ward off this damage entirely.
In the past few years, companies have started marketing drugs that slow Alzheimer’s-related cognitive decline by clearing amyloid from the brain, and scientists have been perfecting highly accurate tests for both amyloid and tau protein.
Researchers call for a major rethink of how Alzheimer’s treatments are evaluated
“It’s this confluence of the possibility of widespread clinically available, accurate diagnosis with the ability to do something about the disease that prompted us to update the criteria,” says Clifford Jack, a specialist in clinical Alzheimer’s and dementia research at Mayo Clinic in Rochester, Minnesota, who co-led the effort to revise the diagnosis criteria. Jack and his colleagues in a working group for the Alzheimer’s Association, a non-profit research and advocacy organization in Chicago, Illinois, published their guidelines2 in the journal Alzheimer’s & Dementia in June.
The criteria say that any one abnormal result on a core set of biomarker-based tests is sufficient to diagnose Alzheimer’s. These tests include measurements of amyloid and tau-protein levels in blood or cerebrospinal fluid, and a positron-emission tomography (PET) brain scan, which helps to quantify amyloid plaques.
Devastating diagnosis
But Villain and his colleagues point out in their critique that a large swathe of people diagnosed in this way would never develop any cognitive symptoms: a 65-year-old man who is amyloid-biomarker positive has a lifetime risk of developing Alzheimer’s dementia of about 22%, which is only roughly 1.7 times higher than the risk for a similar individual who is amyloid-biomarker negative.
The critics also argue that people who test positive for a single biomarker and are cognitively unimpaired should be informed that they are at risk of the disease but should not be given an official Alzheimer’s diagnosis. A person without symptoms who either tests positive on multiple biomarker tests or has a gene variant known to significantly increase the risk of developing Alzheimer’s dementia could be given a diagnosis of ‘presymptomatic’ Alzheimer’s, the critics write.
Landmark Alzheimer’s drug approval confounds research community
Jack acknowledges that biomarker testing makes it possible for asymptomatic individuals to be diagnosed with the disease — but the guidelines state that biologically-based diagnoses are intended to “assist rather than supplant” clinical evaluations. And the working group does not recommend Alzheimer’s biomarker tests for healthy people, so a hypothetical positive diagnosis for someone without symptoms should not come to pass, he says.
However, the new criteria might expand eligibility for clinical trials, which could help to develop treatments for asymptomatic individuals, Jack says. “The reality is that every person who ultimately becomes demented due to Alzheimer’s went through a period of time when they were asymptomatic with the disease,” he says. “Medicine needs to focus its future on how to prevent the onset of symptoms, because by the time someone becomes symptomatic, extensive irreversible damage has already occurred.”
Nothing in the cupboard
But medications for biomarker-positive, asymptomatic people are currently non-existent except in clinical trials, says Andrea Bozoki, a cognitive neurologist at the University of North Carolina School of Medicine in Chapel Hill who co-wrote the JAMA Neurology critique. This would leave such people with the mental anguish of having a diagnosis for an incurable disease but lacking treatment options, she says.
The new drugs that that slow the cognitive decline caused by the disease are approved in the United States only for people who are already experiencing mild cognitive impairment.
Bozoki worries that the new criteria will spur healthy people who fear that they are at risk for Alzheimer’s, or who have a family history of the disease, to find a doctor who will order a biomarker test for them. And if they’re diagnosed, she says, they might be prescribed the new Alzheimer’s drugs. These haven’t been shown to be effective in asymptomatic populations, cost tens of thousands of US dollars a year and carry a risk of brain bleeding and fatal seizures.
This will make it even more important for researchers and doctors to ensure that they are properly communicating risk and uncertainty as Alzheimer’s tests and drugs become more available, says Winston Chiong, a neurologist and ethicist at the University of California, San Francisco, who was not involved with either workgroup.