Flaumenhaft, R., Enjyoji, K. & Schmaier, A. A. Vasculopathy in COVID-19. Blood 140, 222–235 (2022).
Conway, E. M. et al. Understanding COVID-19-associated coagulopathy. Nat. Rev. Immunol. 22, 639–649 (2022).
Mentzer, S. J., Ackermann, M. & Jonigk, D. Endothelialitis, microischemia, and intussusceptive angiogenesis in COVID-19. Cold Spring Harb. Perspect. Med. 12, a041157 (2022).
Ahamed, J. & Laurence, J. Long COVID endotheliopathy: hypothesized mechanisms and potential therapeutic approaches. J. Clin. Invest. 132, e161167 (2022).
Osiaevi, I. et al. Persistent capillary rarefication in long COVID syndrome. Angiogenesis 26, 53–61 (2023).
Rovas, A. et al. Microvascular dysfunction in COVID-19: the MYSTIC study. Angiogenesis 24, 145–157 (2021).
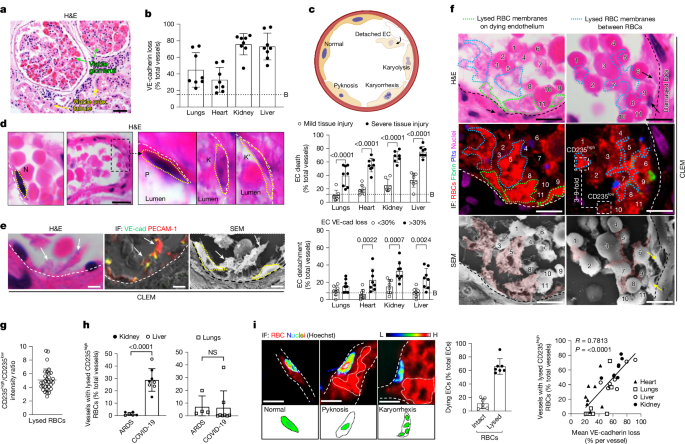
Ackermann, M. et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in COVID-19. N. Engl. J. Med. 383, 120–128 (2020).
Heinrich, F., Mertz, K. D., Glatzel, M., Beer, M. & Krasemann, S. Using autopsies to dissect COVID-19 pathogenesis. Nat. Microbiol. 8, 1986–1994 (2023).
Mackman, N., Antoniak, S., Wolberg, A. S., Kasthuri, R. & Key, N. S. Coagulation abnormalities and thrombosis in patients infected with SARS-CoV-2 and other pandemic viruses. Arterioscler. Thromb. Vasc. Biol. 40, 2033–2044 (2020).
Rapkiewicz, A. V. et al. Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. eClinicalMedicine 24, 100434 (2020).
Bonaventura, A. et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat. Rev. Immunol. 21, 319–329 (2021).
Lupu, L., Palmer, A. & Huber-Lang, M. Inflammation, thrombosis, and destruction: the three-headed Cerberus of trauma- and SARS-CoV-2-induced ARDS. Front. Immunol. 11, 584514 (2020).
Marchi, G. et al. Red blood cell morphologic abnormalities in patients hospitalized for COVID-19. Front. Physiol. 13, 932013 (2022).
Johansson, P. I., Stensballe, J. & Ostrowski, S. R. Shock induced endotheliopathy (SHINE) in acute critical illness—a unifying pathophysiologic mechanism. Crit. Care 21, 25 (2017).
Stegmayr, B., Abdel-Rahman, E. M. & Balogun, R. A. Septic shock with multiorgan failure: from conventional apheresis to adsorption therapies. Semin. Dial. 25, 171–175 (2012).
Aguado, J. et al. Senolytic therapy alleviates physiological human brain aging and COVID-19 neuropathology. Nat. Aging 3, 1561–1575 (2023).
Albornoz, E. A. et al. SARS-CoV-2 drives NLRP3 inflammasome activation in human microglia through spike protein. Mol. Psychiatry 28, 2878–2893 (2023).
Xu, G. et al. SARS-CoV-2 promotes RIPK1 activation to facilitate viral propagation. Cell Res. 31, 1230–1243 (2021).
Wang, C., Wang, Z., Allen, R., Bishop, G. A. & Sharland, A. F. A modified method for heterotopic mouse heart transplantion. J. Vis. Exp. https://doi.org/10.3791/51423 (2014).
Choi, M. E., Price, D. R., Ryter, S. W. & Choi, A. M. K. Necroptosis: a crucial pathogenic mediator of human disease. JCI Insight 4, e128834 (2019).
Winn, R. K. & Harlan, J. M. The role of endothelial cell apoptosis in inflammatory and immune diseases. J. Thromb. Haemost. 3, 1815–1824 (2005).
Bombeli, T., Karsan, A., Tait, J. F. & Harlan, J. M. Apoptotic vascular endothelial cells become procoagulant. Blood 89, 2429–2442 (1997).
Bombeli, T., Schwartz, B. R. & Harlan, J. M. Endothelial cells undergoing apoptosis become proadhesive for nonactivated platelets. Blood 93, 3831–3838 (1999).
Linkermann, A. et al. Two independent pathways of regulated necrosis mediate ischemia-reperfusion injury. Proc. Natl Acad. Sci. USA 110, 12024–12029 (2013).
Pasparakis, M. & Vandenabeele, P. Necroptosis and its role in inflammation. Nature 517, 311–320 (2015).
Nauta, A. J. et al. Mannose-binding lectin engagement with late apoptotic and necrotic cells. Eur. J. Immunol. 33, 2853–2863 (2003).
Navratil, J. S., Watkins, S. C., Wisnieski, J. J. & Ahearn, J. M. The globular heads of C1q specifically recognize surface blebs of apoptotic vascular endothelial cells. J. Immunol. 166, 3231–3239 (2001).
Afzali, B., Noris, M., Lambrecht, B. N. & Kemper, C. The state of complement in COVID-19. Nat. Rev. Immunol. 22, 77–84 (2022).
Conway, E. M. & Pryzdial, E. L. G. Is the COVID-19 thrombotic catastrophe complement-connected? J. Thromb. Haemost. 18, 2812–2822 (2020).
Magro, C. et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl. Res. 220, 1–13 (2020).
Niederreiter, J. et al. Complement activation via the lectin and alternative pathway in patients with severe COVID-19. Front. Immunol. 13, 835156 (2022).
Kolb, W. P., Haxby, J. A., Arroyave, C. M. & Muller-Eberhard, H. J. Molecular analysis of the membrane attack mechanism of complement. J. Exp. Med. 135, 549–566 (1972).
Keep, R. F. et al. Brain endothelial cell junctions after cerebral hemorrhage: changes, mechanisms and therapeutic targets. J. Cereb. Blood Flow Metab. 38, 1255–1275 (2018).
Scarabelli, T. et al. Apoptosis of endothelial cells precedes myocyte cell apoptosis in ischemia/reperfusion injury. Circulation 104, 253–256 (2001).
Etulain, J. et al. Acidosis downregulates platelet haemostatic functions and promotes neutrophil proinflammatory responses mediated by platelets. Thromb. Haemost. 107, 99–110 (2012).
Meng, Z. H., Wolberg, A. S., Monroe, D. M. 3rd & Hoffman, M. The effect of temperature and pH on the activity of factor VIIa: implications for the efficacy of high-dose factor VIIa in hypothermic and acidotic patients. J. Trauma 55, 886–891 (2003).
Ataga, K. I. et al. Crizanlizumab for the prevention of pain crises in sickle cell disease. N. Engl. J. Med. 376, 429–439 (2017).
Liu, W. et al. RGMb protects against acute kidney injury by inhibiting tubular cell necroptosis via an MLKL-dependent mechanism. Proc. Natl Acad. Sci. USA 115, E1475–E1484 (2018).
Stempien-Otero, A. et al. Mechanisms of hypoxia-induced endothelial cell death: role of p53 in apoptosis. J. Biol. Chem. 274, 8039–8045 (1999).
Uria-Avellanal, C. & Robertson, N. J. Na+/H+ exchangers and intracellular pH in perinatal brain injury. Transl. Stroke Res. 5, 79–98 (2014).
Kenawy, H. I., Boral, I. & Bevington, A. Complement-coagulation cross-talk: a potential mediator of the physiological activation of complement by low pH. Front. Immunol. 6, 215 (2015).
Akhter, N. et al. Impact of COVID-19 on the cerebrovascular system and the prevention of RBC lysis. Eur. Rev. Med. Pharmacol. Sci. 24, 10267–10278 (2020).
Bouchla, A. et al. Red blood cell abnormalities as the mirror of SARS-CoV-2 disease severity: a pilot study. Front. Physiol. 12, 825055 (2021).
Cervia-Hasler, C. et al. Persistent complement dysregulation with signs of thromboinflammation in active long Covid. Science 383, eadg7942 (2024).
Kloner, R. A., King, K. S. & Harrington, M. G. No-reflow phenomenon in the heart and brain. Am. J. Physiol. Heart Circ. Physiol. 315, H550–H562 (2018).
Zille, M. et al. The impact of endothelial cell death in the brain and its role after stroke: a systematic review. Cell Stress 3, 330–347 (2019).
Li, Y. et al. Myeloid-derived MIF drives RIPK1-mediated cerebromicrovascular endothelial cell death to exacerbate ischemic brain injury. Proc. Natl Acad. Sci. USA 120, e2219091120 (2023).
Wenzel, J. et al. The SARS-CoV-2 main protease Mpro causes microvascular brain pathology by cleaving NEMO in brain endothelial cells. Nat. Neurosci. 24, 1522–1533 (2021).
Niccoli, G., Scalone, G., Lerman, A. & Crea, F. Coronary microvascular obstruction in acute myocardial infarction. Eur. Heart J. 37, 1024–1033 (2016).
Murphy, J. M. et al. The pseudokinase MLKL mediates necroptosis via a molecular switch mechanism. Immunity 39, 443–453 (2013).
Yap, C. L. et al. Synergistic adhesive interactions and signaling mechanisms operating between platelet glycoprotein Ib/IX and integrin αIIbβ3. J. Biol. Chem. 275, 41377–41388 (2000).
Wu, M. C. et al. The receptor for complement component C3a mediates protection from intestinal ischemia-reperfusion injuries by inhibiting neutrophil mobilization. Proc. Natl Acad. Sci. USA 110, 9439–9444 (2013).
Yuan, Y. et al. Neutrophil macroaggregates promote widespread pulmonary thrombosis after gut ischemia. Sci. Transl. Med. 9, eaam5861 (2017).
Maclean, J. A. A. et al. Development of a carotid artery thrombolysis stroke model in mice. Blood Adv. 6, 5449–5462 (2022).
Bialkowska, A. B., Ghaleb, A. M., Nandan, M. O. & Yang, V. W. Improved Swiss-rolling technique for intestinal tissue preparation for immunohistochemical and immunofluorescent analyses. J. Vis. Exp. https://doi.org/10.3791/54161 (2016).
Chiu, C. J., McArdle, A. H., Brown, R., Scott, H. J. & Gurd, F. N. Intestinal mucosal lesion in low-flow states. I. A morphological, hemodynamic, and metabolic reappraisal. Arch. Surg. 101, 478–483 (1970).
Shami, G. J. et al. 3-D EM exploration of the hepatic microarchitecture—lessons learned from large-volume in situ serial sectioning. Sci. Rep. 6, 36744 (2016).
Strilic, B. et al. Tumour-cell-induced endothelial cell necroptosis via death receptor 6 promotes metastasis. Nature 536, 215–218 (2016).
Majno, G. & Joris, I. Apoptosis, oncosis, and necrosis. An overview of cell death. Am. J. Pathol. 146, 3–15 (1995).
Gujral. J. S., Knight, T. R., Farhood, A., Bajt, M. L. & Jaeschke. H. Mode of cell death after acetaminophen overdose in mice: apoptosis or oncotic necrosis? Toxicol. Sci. 67, 322–388 (2002).