Ho, J. Y. Life course patterns of prescription drug use in the United States. Demography 60, 1549–1579 (2023).
Weersma, R. K., Zhernakova, A. & Fu, J. Interaction between drugs and the gut microbiome. Gut 69, 1510–1519 (2020).
Caruso, R., Lo, B. C. & Núñez, G. Host–microbiota interactions in inflammatory bowel disease. Nat. Rev. Immunol. 20, 411–426 (2020).
Dehner, C., Fine, R. & Kriegel, M. A. The microbiome in systemic autoimmune disease: mechanistic insights from recent studies. Curr. Opin. Rheumatol. 31, 201–207 (2019).
Wong, S. H. & Yu, J. Gut microbiota in colorectal cancer: mechanisms of action and clinical applications. Nat. Rev. Gastroenterol. Hepatol. 16, 690–704 (2019).
Khosravi, A. & Mazmanian, S. K. Disruption of the gut microbiome as a risk factor for microbial infections. Curr. Opin. Microbiol. 16, 221–227 (2013).
Lassalle, M., Zureik, M. & Dray-Spira, R. Proton pump inhibitor use and risk of serious infections in young children. JAMA Pediatr. 177, 1028–1038 (2023).
Roberts, M. B. & Fishman, J. A. Immunosuppressive agents and infectious risk in transplantation: managing the “net state of immunosuppression”. Clin. Infect. Dis. 73, e1302–e1317 (2021).
Budnitz, D. S., Lovegrove, M. C., Shehab, N. & Richards, C. L. Emergency hospitalizations for adverse drug events in older Americans. New Engl. J. Med. 365, 2002–2012 (2011).
Maier, L. et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 555, 623–628 (2018).
Vich Vila, A. et al. Impact of commonly used drugs on the composition and metabolic function of the gut microbiota. Nat. Commun. 11, 362 (2020).
Zimmermann, M., Zimmermann-Kogadeeva, M., Wegmann, R. & Goodman, A. L. Mapping human microbiome drug metabolism by gut bacteria and their genes. Nature 570, 462–467 (2019).
Verdegaal, A. A. & Goodman, A. L. Integrating the gut microbiome and pharmacology. Sci. Transl. Med. 16, eadg8357 (2024).
Zhong, W. et al. Age and sex patterns of drug prescribing in a defined American population. Mayo Clin. Proc. 88, 697–707 (2013).
Hales, C. M., Servais, J., Martin, C. B. & Kohen, D. Prescription Drug Use Among Adults Aged 40–79 in the United States and Canada. NCHS Data Brief No. 347 (NCHS, 2019).
Kyu, H. H. et al. Global, regional, and national age-sex-specific burden of diarrhoeal diseases, their risk factors, and aetiologies, 1990–2021, for 204 countries and territories: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Infect. Dis. 25, 519–536 (2025).
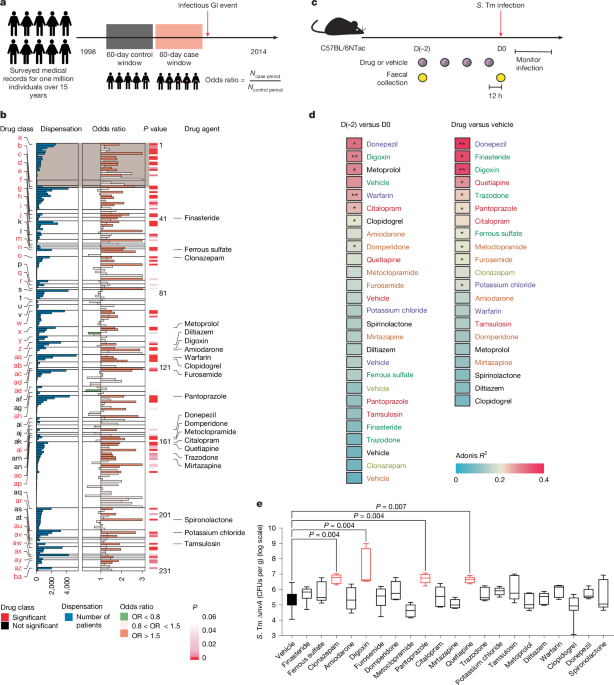
Jaakkola, J. J. K. Case-crossover design in air pollution epidemiology. Eur. Respir. J. 21, 81s–85s (2003).
Bohnhoff, M., Drake, B. L. & Miller, C. P. Effect of streptomycin on susceptibility of intestinal tract to experimental Salmonella infection. Proc. Soc. Exp. Biol. Med. 86, 132–137 (1954).
Galán, J. E. Salmonella Typhimurium and inflammation: a pathogen-centric affair. Nat. Rev. Microbiol. 19, 716–725 (2021).
Wagner, S. et al. Organization and coordinated assembly of the type III secretion export apparatus. Proc. Natl Acad. Sci. USA 107, 17745–17750 (2010).
Dobkin, J. F., Saha, J. R., Butler, V. P., Neu, H. C. & Lindenbaum, J. Digoxin-inactivating bacteria: identification in human gut flora. Science 220, 325–327 (1983).
Haiser, H. J. et al. Predicting and manipulating cardiac drug inactivation by the human gut bacterium Eggerthella lenta. Science 341, 295–298 (2013).
Hackam, D. J. et al. Host resistance to intracellular infection: mutation of natural resistance-associated macrophage protein 1 (Nramp1) impairs phagosomal acidification. J. Exp. Med. 188, 351–364 (1998).
Huh, J. R. et al. Digoxin and its derivatives suppress TH17 cell differentiation by antagonizing RORγt activity. Nature 472, 486–490 (2011).
Xiao, S. et al. Small-molecule RORγt antagonists inhibit T helper 17 cell transcriptional network by divergent mechanisms. Immunity 40, 477–489 (2014).
Spits, H. et al. Innate lymphoid cells—a proposal for uniform nomenclature. Nat. Rev. Immunol. 13, 145–149 (2013).
Ivanov, I. I. et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell 139, 485–498 (2009).
Zindl, C. L. et al. IL-22-producing neutrophils contribute to antimicrobial defense and restitution of colonic epithelial integrity during colitis. Proc. Natl Acad. Sci. USA 110, 12768–12773 (2013).
Flannigan, K. L. et al. IL-17A-mediated neutrophil recruitment limits expansion of segmented filamentous bacteria. Mucosal Immunol. 10, 673–684 (2017).
Raffatellu, M. et al. Simian immunodeficiency virus-induced mucosal interleukin-17 deficiency promotes Salmonella dissemination from the gut. Nat. Med. 14, 421–428 (2008).
Ivanov, I. I., Tuganbaev, T., Skelly, A. N. & Honda, K. T cell responses to the microbiota. Annu. Rev. Immunol. 40, 559–587 (2022).
Araujo, L. P. et al. Context-dependent role of group 3 innate lymphoid cells in mucosal protection. Sci. Immunol. 9, eade7530 (2024).
Salzman, N. H. et al. Enteric defensins are essential regulators of intestinal microbial ecology. Nat. Immunol. 11, 76–83 (2010).
Vaishnava, S. et al. The antibacterial lectin RegIIIγ promotes the spatial segregation of microbiota and host in the intestine. Science 334, 255–258 (2011).
Jonsson, H., Hugerth, L. W., Sundh, J., Lundin, E. & Andersson, A. F. Genome sequence of segmented filamentous bacteria present in the human intestine. Commun. Biol. 3, 485 (2020).
Atarashi, K. et al. Th17 cell induction by adhesion of microbes to intestinal epithelial cells. Cell 163, 367–380 (2015).
Raffatellu, M. et al. Lipocalin-2 resistance of Salmonella enterica serotype Typhimurium confers an advantage during life in the inflamed intestine. Cell Host Microbe 5, 476 (2009).
Pazgier, M., Hoover, D. M., Yang, D., Lu, W. & Lubkowski, J. Human β-defensins. Cell. Mol. Life Sci. 63, 1294–1313 (2006).
Frye, M., Bargon, J., Lembcke, B., Wagner, T. O. & Gropp, R. Differential expression of human α- and β-defensins mRNA in gastrointestinal epithelia. Eur. J. Clin. Invest. 30, 695–701 (2000).
Semple, F. & Dorin, J. R. β-Defensins: multifunctional modulators of infection, inflammation and more? J. Innate Immun. 4, 337–348 (2012).
Salzman, N. H., Underwood, M. A. & Bevins, C. L. Paneth cells, defensins, and the commensal microbiota: a hypothesis on intimate interplay at the intestinal mucosa. Semin. Immunol. 19, 70–83 (2007).
Rezende, R. M. & Weiner, H. L. History and mechanisms of oral tolerance. Semin. Immunol. 30, 3–11 (2017).
Rivas, M. N. & Chatila, T. A. Regulatory T cells in allergic diseases. J. Allergy Clin. Immunol. 138, 639–652 (2016).
Kongkaew, C., Sakunrag, I. & Jianmongkol, P. Non-compliance with digoxin in patients with heart failure and/or atrial fibrillation: a systematic review and meta-analysis of observational studies. Arch. Cardiovasc. Dis. 105, 507–516 (2012).
Dearing, M. D. & Weinstein, S. B. Metabolic enabling and detoxification by mammalian gut microbes. Annu. Rev. Microbiol. 76, 579–596 (2022).
Chiu, K., Warner, G., Nowak, R. A., Flaws, J. A. & Mei, W. The impact of environmental chemicals on the gut microbiome. Toxicol. Sci. 176, 253–284 (2020).
Rothschild, D. et al. Environment dominates over host genetics in shaping human gut microbiota. Nature 555, 210–215 (2018).
David, L. A. et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 505, 559–563 (2014).
Bäumler, A. J. & Sperandio, V. Interactions between the microbiota and pathogenic bacteria in the gut. Nature 535, 85–93 (2016).
Woodward, M. Epidemiology: Study Design and Data Analysis 3rd edn (CRC Press, 2013).
Hou, J. et al. Temporal trends in clinical evidence of 5-year survival within electronic health records among patients with early-stage colon cancer managed with laparoscopy-assisted colectomy vs open colectomy. JAMA Netw. Open 5, e2218371 (2022).
Corrigan-Curay, J., Sacks, L. & Woodcock, J. Real-world evidence and real-world data for evaluating drug safety and effectiveness. JAMA 320, 867–868 (2018).
Fralick, M., Kesselheim, A. S., Avorn, J. & Schneeweiss, S. Use of health care databases to support supplemental indications of approved medications. JAMA Intern. Med. 178, 55–63 (2018).
Pletcher, M. J. et al. Randomized controlled trials of electronic health record interventions: design, conduct, and reporting considerations. Ann. Intern. Med. 172, S85–S91 (2020).
Lewer, D. et al. Fatal opioid overdoses during and shortly after hospital admissions in England: a case-crossover study. PLoS Med. 18, e1003759 (2021).
Shuto, H. et al. Medication use as a risk factor for inpatient falls in an acute care hospital: a case-crossover study. Br. J. Clin. Pharmacol. 69, 535–542 (2010).
Pindyck, T. et al. Validation of acute gastroenteritis-related international classification of diseases, clinical modification codes in pediatric and adult US populations. Clin. Infect. Dis. 70, 2423–2427 (2020).
Cadieux, G. et al. Accuracy of syndrome definitions based on diagnoses in physician claims. BMC Public Health 11, 17 (2011).
Gu, Z., Eils, R. & Schlesner, M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics 32, 2847–2849 (2016).
Goodman, A. L. et al. Identifying genetic determinants needed to establish a human gut symbiont in its habitat. Cell Host Microbe 6, 279–289 (2009).
King, A. M. et al. Aspergillomarasmine A overcomes metallo-β-lactamase antibiotic resistance. Nature 510, 503–506 (2014).
Kolde, R. pheatmap: Pretty heatmaps. R package v.1.0.12 (CRAN, 2019).
Wotzka, S. Y. et al. Escherichia coli limits Salmonella Typhimurium infections after diet shifts and fat-mediated microbiota perturbation in mice. Nat. Microbiol. 4, 2164–2174 (2019).
Velazquez, E. M. et al. Endogenous Enterobacteriaceae underlie variation in susceptibility to Salmonella infection. Nat. Microbiol. 4, 1057–1064 (2019).
Hoiseth, S. K. & Stocker, B. A. Aromatic-dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature 291, 238–239 (1981).
Caballero-Flores, G., Pickard, J. M., Fukuda, S., Inohara, N. & Núñez, G. An enteric pathogen subverts colonization resistance by evading competition for amino acids in the gut. Cell Host Microbe 28, 526–533 (2020).
Zhao, P. et al. Digoxin improves steatohepatitis with differential involvement of liver cell subsets in mice through inhibition of PKM2 transactivation. Am. J. Physiol. Gastrointest. Liver Physiol. 317, G387–G397 (2019).
Teijeiro, A., Garrido, A., Ferre, A., Perna, C. & Djouder, N. Inhibition of the IL-17A axis in adipocytes suppresses diet-induced obesity and metabolic disorders in mice. Nat. Metab. 3, 496–512 (2021).
Patel, S., Preuss, C. V. & Bernice, F. in StatPearls https://www.ncbi.nlm.nih.gov/books/NBK459263/ (StatPearls Publishing, 2024).
Sun, H., Kamanova, J., Lara-Tejero, M. & Galán, J. E. A family of Salmonella type III secretion effector proteins selectively targets the NF-κB signaling pathway to preserve host homeostasis. PLoS Pathog. 12, e1005484 (2016).
Sun, Z. et al. Requirement for RORγ in thymocyte survival and lymphoid organ development. Science 288, 2369–2373 (2000).
Mombaerts, P. et al. RAG-1-deficient mice have no mature B and T lymphocytes. Cell 68, 869–877 (1992).
Madison, B. B. et al. Cis elements of the villin gene control expression in restricted domains of the vertical (crypt) and horizontal (duodenum, cecum) axes of the intestine. J. Biol. Chem. 277, 33275–33283 (2002).
Behringer, R. Manipulating the Mouse Embryo: A Laboratory Manual (Cold Spring Harbor Laboratory Press, 2014).
Meade, K. G. & O’Farrelly, C. β-Defensins: farming the microbiome for homeostasis and health. Front. Immunol. 9, 3072 (2019).
Horvat, B., Osborn, M. & Damjanov, I. Expression of villin in the mouse oviduct and the seminiferous ducts. Histochemistry 93, 661–663 (1990).
Rutlin, M. et al. The Villin1 gene promoter drives Cre recombinase expression in extraintestinal tissues. Cell. Mol. Gastroenterol. Hepatol. 10, 864–867 (2020).
Kaminski, J. et al. High-specificity targeted functional profiling in microbial communities with ShortBRED. PLoS Comput. Biol. 11, e1004557 (2015).
Suzek, B. E., Wang, Y., Huang, H., McGarvey, P. B. & Wu, C. H. UniRef clusters: a comprehensive and scalable alternative for improving sequence similarity searches. Bioinformatics 31, 926–932 (2015).
Edgar, R. C. Search and clustering orders of magnitude faster than BLAST. Bioinformatics 26, 2460–2461 (2010).
Tawk, C. et al. Infection leaves a genetic and functional mark on the gut population of a commensal bacterium. Cell Host Microbe 31, 811–826 (2023).
Kuznetsov, D. et al. OrthoDB v11: annotation of orthologs in the widest sampling of organismal diversity. Nucleic Acids Res. 51, D445–D451 (2023).
Yan, K. et al. Obeticholic acid decreases intestinal content of Enterococcus in rats with cirrhosis and ascites. Hepatol. Commun. 5, 1507–1517 (2021).
Kozich, J. J., Westcott, S. L., Baxter, N. T., Highlander, S. K. & Schloss, P. D. Development of a dual-index sequencing strategy and curation pipeline for analyzing amplicon sequence data on the miseq illumina sequencing platform. Appl. Environ. Microbiol. 79, 5112–5120 (2013).
Bolyen, E. et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat. Biotechnol. 37, 852–857 (2019).
Callahan, B. J. et al. DADA2: high-resolution sample inference from Illumina amplicon data. Nat. Methods 13, 581–583 (2016).
Ii, M. S. R. et al. RESCRIPt: reproducible sequence taxonomy reference database management. PLoS Comput. Biol. 17, e1009581 (2021).
Pruesse, E. et al. SILVA: a comprehensive online resource for quality checked and aligned ribosomal RNA sequence data compatible with ARB. Nucleic Acids Res. 35, 7188–7196 (2007).
Quast, C. et al. The SILVA ribosomal RNA gene database project: improved data processing and web-based tools. Nucleic Acids Res. 41, D590–D596 (2013).
Fernandes, A. D. et al. Unifying the analysis of high-throughput sequencing datasets: characterizing RNA-seq, 16S rRNA gene sequencing and selective growth experiments by compositional data analysis. Microbiome 2, 15 (2014).
Lozupone, C. A., Hamady, M., Kelley, S. T. & Knight, R. Quantitative and qualitative β diversity measures lead to different insights into factors that structure microbial communities. Appl. Environ. Microbiol. 73, 1576–1585 (2007).
Oksanen, J. et al. vegan: Community ecology package. R package v.2.6-4 (CRAN, 2024).
Liu, Y.-X. et al. EasyAmplicon: an easy-to-use, open-source, reproducible, and community-based pipeline for amplicon data analysis in microbiome research. iMeta 2, e83 (2023).
Kumar, A. et al. The serotonin neurotransmitter modulates virulence of enteric pathogens. Cell Host Microbe 28, 41–53 (2020).
Kim, D., Paggi, J. M., Park, C., Bennett, C. & Salzberg, S. L. Graph-based genome alignment and genotyping with HISAT2 and HISAT-genotype. Nat. Biotechnol. 37, 907–915 (2019).
Pertea, M. et al. StringTie enables improved reconstruction of a transcriptome from RNA-seq reads. Nat. Biotechnol. 33, 290–295 (2015).
Love, M. I., Huber, W. & Anders, S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 15, 550 (2014).
Milacic, M. et al. The Reactome Pathway Knowledgebase 2024. Nucleic Acids Res. 52, D672–D678 (2023).
Castanza, A. S. et al. Extending support for mouse data in the Molecular Signatures Database (MSigDB). Nat. Methods 20, 1619–1620 (2023).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).