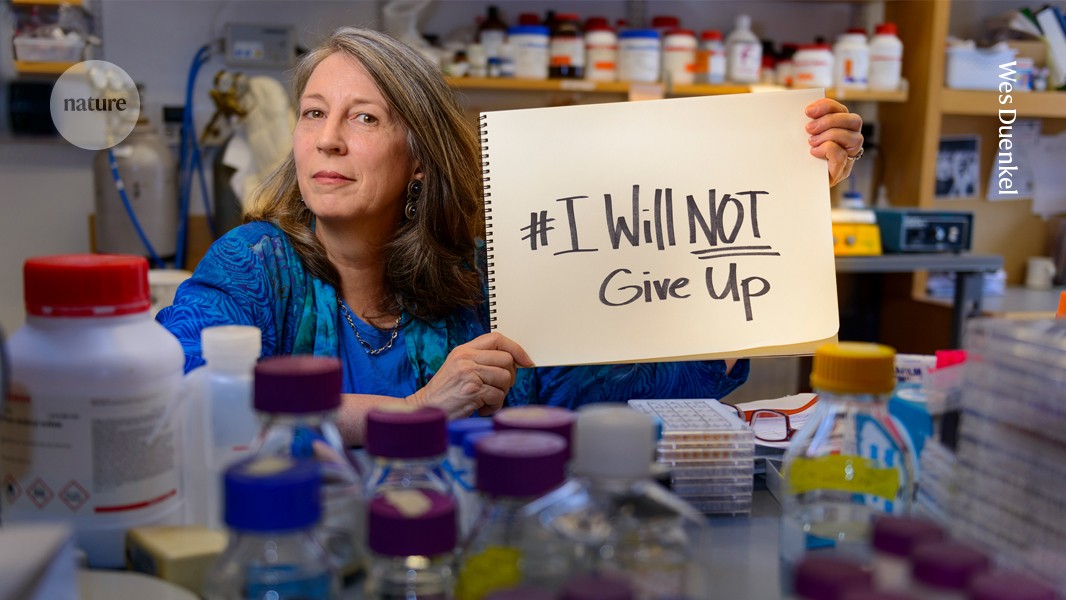
Terry Jo Bichell (pictured in her laboratory) was part of a 2016 campaign in which scientists shared their inspirational stories.Credit: Wes Duenkel
Terry Jo Bichell sensed there was something different about her fifth, youngest child when he was just a baby. At first, doctors and friends told her that she was being neurotic, that there was nothing wrong. But when the boy, Lou, couldn’t sit up properly at the age of one, a paediatrician decided to run some tests.
A blood test revealed that Lou had Angelman syndrome, a rare developmental disorder with symptoms such as impaired motor function, limited or no speech, seizures and difficulty in sleeping. It affects one in 12,000 to one in 20,000 individuals, and there is no known cure.
Bichell heard about this diagnosis in 2000 in San Miguel de Allende, Mexico, where she was teaching at a midwifery school at the time. She remembers that, soon after, she walked half an hour to get to an Internet-connected computer to learn more.
But merely reading about Angelman syndrome didn’t satisfy Bichell. She wanted to help to find a cure, or at least a treatment — even if it meant becoming a scientist herself.
In July 2000, Bichell flew to Finland with her mother and the baby to attend the first major international conference on Angelman syndrome in Tampere. “It was the first time I had really been interested in hard science” as opposed to health care, Bichell remembers. “And it was just fascinating. And it felt like we were on the verge of a treatment, and all we had to do was just reach through the curtain, and we’d be able to figure it out.”
Sleepless nights
Angelman syndrome is named after British physician Harry Angelman, who, in 1965, noted three children with poor muscle control and abnormalities of the brain, skull and eyes, and who frequently laughed. It wasn’t until the late 1990s that scientists identified a mutation in the UBE3A gene, on chromosome 15, as the cause. Most people have both maternal and paternal copies of UBE3A, and the condition is most commonly the result of the maternal copy being absent or damaged. Overexpression of a protein linked to the same gene has been linked to autism spectrum disorders1.
At the Tampere conference, Lou’s sleep challenges were exacerbated by jet lag and the long daylight hours near the Arctic Circle, and Bichell would do 3 a.m. walks with him in the hotel lobby. That’s how she got to know Arthur Beaudet, a geneticist at Baylor College of Medicine in Houston, Texas, who helped to establish the connection between Angelman syndrome and UBE3A. Beaudet found himself sleepless at the same time, and the two of them discussed starting a clinical trial in San Diego, California, where Bichell was then based. The idea was to test supplements called folate and betaine as possible treatments for Angelman syndrome, on the basis that these substances might lessen some of the symptoms. Although the trial proved unsuccessful, it led to Bichell becoming a coordinator and part-time co-investigator for research into the condition.
At that point, Bichell hadn’t trained in medicine, genetics or neurobiology. She had, at first, worked as a documentary film-maker, but her career aspirations changed during a film shoot in Côte d’Ivoire in 1986, when she saw a baby die after a difficult birth. The experience made her determined to become a midwife, and subsequent degrees in nursing and public health equipped her for her new calling.
In 2000, Bichell partnered with Lynne Bird, a clinical geneticist at Rady Children’s Hospital in San Diego, to raise funds for and undertake Angelman research projects, including the folic acid and betaine trials. In a subsequent study on the natural course of the condition, Bichell interviewed more than 100 families of children with Angelman, work that she continued at Vanderbilt University after her family moved to Nashville, Tennessee, in 2006.
Lou’s sleep difficulties persisted, and Bichell remembers feeling sleep-deprived herself while driving to Vanderbilt to teach pre-literacy skills to children with Angelman. She began to wonder whether the circadian system had some connection to the disorder. “I didn’t think that anyone else in the world would be interested in following up on those hunches,” she says.
Biology homework
Eventually, Bichell decided she couldn’t sit back and await developments that might help Lou. She resolved to train as a neuroscientist and, one day, to determine the direction of research herself. “I was almost 40 when he was born, and that meant that I was probably going to die 40 years before him,” she says. This meant that “somebody else was going to have to take care of him all that time”, so she felt she had better find a treatment for the condition.
Aged 49, she enrolled in a neuroscience PhD programme at Vanderbilt in 2009 and found herself doing homework alongside her teenage daughters, who were also studying biology.
Initially, Bichell worked in a laboratory specializing in Angelman syndrome. But when the principal investigator decided to quit research, she lost her funding to probe the very condition that she had set out to study.
To stay in the programme, she would need to redirect her energy to a topic she knew nothing about for her dissertation. So, Bichell joined the lab of neuroscientist Aaron Bowman to work on Huntington’s disease, an inherited neurodegenerative condition. In retrospect, she appreciates the shift. “It expanded my mind beyond just Angelman syndrome, so then I was able to learn about a lot of other disorders and think more globally,” she says.
But the question of how the circadian system plays a role in Angelman continued to nag at Bichell. At Vanderbilt, she found an ally in Carl Johnson, who specializes in studies of circadian rhythms but knew little about Angelman syndrome. “She basically sucked me into this,” he says. Johnson had a small grant to support her investigations, which led to peer-reviewed papers demonstrating links between circadian rhythms and the condition2.
Being a PhD student in her fifties came with challenges. Whereas most graduate students could check on their experiments in the evenings, Bichell needed to pick up her children from school, take them to sporting events and cook their meals. (Lou attended Nashville public schools with the help of an educational assistant.) She would sometimes set an alarm in the middle of the night so that she could have uninterrupted research time on campus. “I would be there in the dark with all those creepy lab sounds going on, and nobody else there,” she says.
One night in 2010, while 11-year-old Lou, his father and two of his sisters slumbered at home, Bichell found herself crying in the lab, unable to wipe her tears off her nose because her hands were in a sterile area. “I just felt like, ‘This is horrible. What am I doing to my family? What am I doing to myself?’”
The mini-lab manager
But Birchell’s schedule became more sustainable when she created what she called a “mini-lab” of undergraduate students to work and study with her. Just as a principal investigator would, she delegated a host of small tasks to the students, but remained in charge of the experiments and analysis. The group learnt as a collective, rather than competing with one another.
“I felt like I was a mum to all my students and grad students. I was feeding the kids dinner, and then I was going back to the lab and feeding the cells,” she says. “It was all the same”, she laughs, just on “a slightly different scale”.
For her dissertation, Bichell investigated the role of manganese — which is essential for cells and yet toxic when overabundant— in mouse models of Huntington’s disease3. Exposing the mice to supplemental manganese led to a rebalancing of the natural urea cycle, a crucial process that mediates ammonia’s removal from the bloodstream. Her findings support the idea that the mutation in HTT, the gene that causes Huntington’s, leads to a deficiency of manganese in the brain, which contributes to increases in urea and ammonia, also in the brain. More research is needed to determine whether manganese could be involved in treatment, Bowman says.
Bowman, who now heads the School of Life Sciences at Purdue University in West Lafayette, Indiana, remembers the unusually large audience at Bichell’s thesis defence in September 2016, including the many undergraduates who had worked with her, plus faculty members, other graduate students and her family. “She got a standing ovation,” Bowman says. “I have never seen that before. Usually there’s polite clapping.”
Bichell never had expectations of going into academia after her graduation: “There’s no time for me to have a career like that,” she says. Instead, using the broadened perspectives she gained in her PhD work, she founded COMBINEDBrain, a non-profit body that connects patient-advocacy groups with clinicians, researchers and pharmaceutical companies. Its goal is to speed up research on treatments for rare genetic neurological disorders, including Angelman syndrome.
“She’s a bridge-builder,” Bowman says. Bichell’s diverse experience gave her credibility among both researchers and patient-advocacy communities, and “there are very few people in this world that can stand strong on both sides”, he says.
Combining forces
Today, Bichell’s son Lou is 25 years old. His speech is limited to “mama”, “dada” and a few approximations of other words, but he uses about 25 sign-language adaptations. Through an iPad app designed for non-speaking individuals, he can construct short sentences. He cannot be left alone in a room.
Bichell is confident that in her lifetime, a “disease-changing” treatment for Angelman syndrome will be found, and thinks that such a treatment would need to go hand in hand with widespread screening of newborns for the condition. COMBINEDBrain is one player in a large collaboration that plans to undertake a whole-genome sequencing study among infants aged 3–12 months who show signs of neurodevelopmental disorders.
Bichell is also hopeful that gene therapies will improve the quality of life of people with Angelman’s syndrome. Lou is currently taking part in an open-label clinical trial, meaning that participants know whether they are receiving an experimental therapy or a placebo. Bichell’s mother, who helped to look after Lou at the conference in Finland more than two decades ago, now assists with caregiving during the treatments in Boston, Massachusetts.
Now that their other children have grown up and moved away, the Bichell family offers rooms in their home to local musicians, who help out with Lou in exchange. Their farm includes a horse, donkey, chickens and bees. Bichell takes care of her grandchildren and teaches a translational neuroscience course at Vanderbilt. To fit everything in, she sometimes works late at night and sleeps only in short spurts, as she did during her graduate studies.
“I always have ten things going on at one time,” she says. “Eight people living in my house, ten animals to take care of, two careers. That’s the only way I really know how to do things.”