Coles, J. A., Myburgh, E., Brewer, J. M. & McMenamin, P. G. Where are we? The anatomy of the murine cortical meninges revisited for intravital imaging, immunology, and clearance of waste from the brain. Prog. Neurobiol. 156, 107–148 (2017).
Buckley, M. W. & McGavern, D. B. Immune dynamics in the CNS and its barriers during homeostasis and disease. Immunol. Rev. 306, 58–75 (2022).
Alves de Lima, K., Rustenhoven, J. & Kipnis, J. Meningeal immunity and its function in maintenance of the central nervous system in health and disease. Annu. Rev. Immunol. 38, 597–620 (2020).
Zong, C., Yu, X., Liu, J. & Liu, Y. Dural venous sinuses: what we need to know. Curr. Med. Imaging 16, 1259–1270 (2020).
Shapiro, M. et al. Venous anatomy of the central nervous system. Neurosurg. Clin. N. Am. 35, 273–286 (2024).
Fitzpatrick, Z. et al. Gut-educated IgA plasma cells defend the meningeal venous sinuses. Nature 587, 472–476 (2020).
Rustenhoven, J. et al. Functional characterization of the dural sinuses as a neuroimmune interface. Cell 184, 1000–1016.e1027 (2021).
Zanluqui, N. G. & McGavern, D. B. Why do central nervous system barriers host a diverse immune landscape? Trends Immunol. 45, 738–749 (2024).
Rua, R. & McGavern, D. B. Advances in meningeal immunity. Trends Mol. Med. 24, 542–559 (2018).
Betsholtz, C. et al. Advances and controversies in meningeal biology. Nat. Neurosci. 27, 2056–2072 (2024).
Mastorakos, P. & McGavern, D. The anatomy and immunology of vasculature in the central nervous system. Sci. Immunol. 4, eaav0492 (2019).
Weed, L. H. Studies on cerebro-spinal fluid. no. II: The theories of drainage of cerebro-spinal fluid with an analysis of the methods of investigation. J. Med. Res. 31, 21–49 (1914).
Toriumi, H. et al. Developmental and circulatory profile of the diploic veins. Microvasc. Res. 81, 97–102 (2011).
Castellani, G., Peralta Ramos, J. M. & Schwartz, M. Bridging anatomical gaps between brain and immune system. Trends Immunol. 45, 318–319 (2024).
Yagmurlu, K. et al. A subset of arachnoid granulations in humans drain to the venous circulation via intradural lymphatic vascular channels. J. Neurosurg. 136, 917–926 (2022).
Shah, T. et al. Arachnoid granulations are lymphatic conduits that communicate with bone marrow and dura-arachnoid stroma. J. Exp. Med. 220, e20220618 (2023).
Smyth, L. C. D. et al. Identification of direct connections between the dura and the brain. Nature 627, 165–173 (2024).
Brioschi, S. et al. Heterogeneity of meningeal B cells reveals a lymphopoietic niche at the CNS borders. Science 373, eabf9277 (2021).
Kim, Y. C. et al. Immaturity of immune cells around the dural venous sinuses contributes to viral meningoencephalitis in neonates. Sci. Immunol. 8, eadg6155 (2023).
Amann, L. et al. Extrasinusoidal macrophages are a distinct subset of immunologically active dural macrophages. Sci. Immunol. 9, eadh1129 (2024).
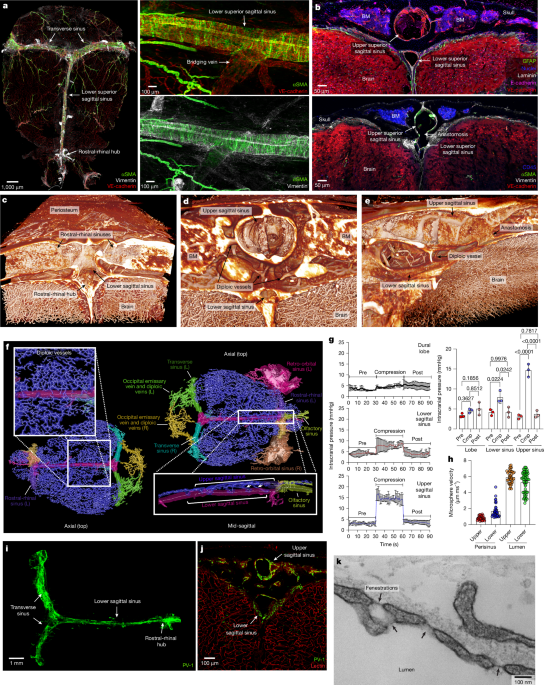
Fitzpatrick, Z. et al. Venous-plexus-associated lymphoid hubs support meningeal humoral immunity. Nature 628, 612–619 (2024).
Louveau, A. et al. Structural and functional features of central nervous system lymphatic vessels. Nature 523, 337–341 (2015).
Aspelund, A. et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J. Exp. Med. 212, 991–999 (2015).
Jacob, L. et al. Conserved meningeal lymphatic drainage circuits in mice and humans. J. Exp. Med. 219, e20220035 (2022).
Herisson, F. et al. Direct vascular channels connect skull bone marrow and the brain surface enabling myeloid cell migration. Nat. Neurosci. 21, 1209–1217 (2018).
Mazzitelli, J. A. et al. Skull bone marrow channels as immune gateways to the central nervous system. Nat. Neurosci. 26, 2052–2062 (2023).
Garcia-Gonzalez, U. et al. The diploic venous system: surgical anatomy and neurosurgical implications. Neurosurg. Focus 27, E2 (2009).
Skrzat, J. & Zarzecki, M. Cranial diploic channels and their veins—a review of literature. Folia Med. Cracov. 62, 77–90 (2022).
Ringstad, G. & Eide, P. K. Cerebrospinal fluid tracer efflux to parasagittal dura in humans. Nat. Commun. 11, 354 (2020).
Epstein, F. H., Mugler, J. P., Cail, W. S. III & Brookeman, J. R. CSF-suppressed T2-weighted three-dimensional MP-RAGE MR imaging. J. Magn. Reson. Imaging 5, 463–469 (1995).
Alarcon-Martinez, L. et al. Capillary pericytes express alpha-smooth muscle actin, which requires prevention of filamentous-actin depolymerization for detection. eLife 7, e34861 (2018).
Pinho-Ribeiro, F. A. et al. Bacteria hijack a meningeal neuroimmune axis to facilitate brain invasion. Nature 615, 472–481 (2023).
Andres, K. H., von During, M., Muszynski, K. & Schmidt, R. F. Nerve fibres and their terminals of the dura mater encephali of the rat. Anat. Embryol. 175, 289–301 (1987).
Zhang, Z., Dickerson, I. M. & Russo, A. F. Calcitonin gene-related peptide receptor activation by receptor activity-modifying protein-1 gene transfer to vascular smooth muscle cells. Endocrinology 147, 1932–1940 (2006).
Scheid, C. R., Honeyman, T. W. & Fay, F. S. Mechanism of β-adrenergic relaxation of smooth muscle. Nature 277, 32–36 (1979).
Tanoue, A. et al. The α1D-adrenergic receptor directly regulates arterial blood pressure via vasoconstriction. J. Clin. Invest. 109, 765–775 (2002).
Sun, Q. et al. Enhancing glymphatic fluid transport by pan-adrenergic inhibition suppresses epileptogenesis in male mice. Nat. Commun. 15, 9600 (2024).
Tanaka, M. et al. The endothelial adrenomedullin-RAMP2 system regulates vascular integrity and suppresses tumour metastasis. Cardiovasc. Res. 111, 398–409 (2016).
Mackay, D. J. & Hall, A. Rho GTPases. J. Biol. Chem. 273, 20685–20688 (1998).
Fischer, J. P., Els-Heindl, S. & Beck-Sickinger, A. G. Adrenomedullin—current perspective on a peptide hormone with significant therapeutic potential. Peptides 131, 170347 (2020).
Kitamura, K. et al. Adrenomedullin: a novel hypotensive peptide isolated from human pheochromocytoma. Biochem. Biophys. Res. Commun. 192, 553–560 (1993).
Santiago, J. A. et al. Comparison of responses to adrenomedullin and adrenomedullin analogs in the mesenteric vascular bed of the cat. Eur. J. Pharmacol. 272, 115–118 (1995).
Pircher, H., Burki, K., Lang, R., Hengartner, H. & Zinkernagel, R. M. Tolerance induction in double specific T-cell receptor transgenic mice varies with antigen. Nature 342, 559–561 (1989).
Walsh, D. R., Lynch, J. J., DT, O. C., Newport, D. T. & Mulvihill, J. J. E. Mechanical and structural characterisation of the dural venous sinuses. Sci. Rep. 10, 21763 (2020).
Oelschlegel, A. M. et al. Beyond the microcirculation: sequestration of infected red blood cells and reduced flow in large draining veins in experimental cerebral malaria. Nat. Commun. 15, 2396 (2024).
Higgins, J. N., Owler, B. K., Cousins, C. & Pickard, J. D. Venous sinus stenting for refractory benign intracranial hypertension. Lancet 359, 228–230 (2002).
Portnoy, H. D., Branch, C. & Castro, M. E. The relationship of intracranial venous pressure to hydrocephalus. Childs Nerv. Syst. 10, 29–35 (1994).
Johnston, I., Kollar, C., Dunkley, S., Assaad, N. & Parker, G. Cranial venous outflow obstruction in the pseudotumour syndrome: incidence, nature and relevance. J. Clin. Neurosci. 9, 273–278 (2002).
Ballabio, E., Valvassori, L., De Simone, R., Bianchi Marzoli, S. & Frediani, F. Idiopathic intracranial hypertension secondary to superior sagittal sinus stenosis: a case report. Neurol. Sci. 45, 5083–5086 (2024).
Schoofs, H. et al. Dynamic cytoskeletal regulation of cell shape supports resilience of lymphatic endothelium. Nature 641, 465–475 (2025).
Kim, J. V., Kang, S. S., Dustin, M. L. & McGavern, D. B. Myelomonocytic cell recruitment causes fatal CNS vascular injury during acute viral meningitis. Nature 457, 191–195 (2009).
Gossa, S., Nayak, D., Zinselmeyer, B. H. & McGavern, D. B. Development of an immunologically tolerated combination of fluorescent proteins for in vivo two-photon imaging. Sci. Rep. 4, 6664 (2014).
Faust, N., Varas, F., Kelly, L. M., Heck, S. & Graf, T. Insertion of enhanced green fluorescent protein into the lysozyme gene creates mice with green fluorescent granulocytes and macrophages. Blood 96, 719–726 (2000).
Zhang, Z. & Zhou, B. Generation of Plvap-CreER and Car4-CreER for genetic targeting of distinct lung capillary populations. J. Genet. Genomics 49, 1093–1100 (2022).
Guo, M. et al. Rapid image deconvolution and multiview fusion for optical microscopy. Nat. Biotechnol. 38, 1337–1346 (2020).
Rosenblum, J. S. et al. Developmental vascular malformations in EPAS1 gain-of-function syndrome. JCI Insight 6, e144368 (2021).
Rosenblum, J. S. et al. Non-invasive in situ visualization of the murine cranial vasculature. Cell Rep. Methods 2, 100151 (2022).
Russo, M. V., Latour, L. L. & McGavern, D. B. Distinct myeloid cell subsets promote meningeal remodeling and vascular repair after mild traumatic brain injury. Nat. Immunol. 19, 442–452 (2018).
Kleinfeld, D., Mitra, P. P., Helmchen, F. & Denk, W. Fluctuations and stimulus-induced changes in blood flow observed in individual capillaries in layers 2 through 4 of rat neocortex. Proc. Natl Acad. Sci. USA 95, 15741–15746 (1998).