Yang, C. et al. Immunoglobulin A antibody composition is sculpted to bind the self gut microbiome. Sci. Immunol. 7, eabg3208 (2022).
Parida, S. et al. A procarcinogenic colon microbe promotes breast tumorigenesis and metastatic progression and concomitantly activates notch and β-catenin axes. Cancer Discov. 11, 1138â1157 (2021).
Arthur, J. C. et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science 338, 120â123 (2012).
Britton, G. J. et al. Defined microbiota transplant restores Th17/RORγt+ regulatory Tâcell balance in mice colonized with inflammatory bowel disease microbiotas. Proc Natl Acad. Sci. USA 117, 21536â21545 (2020).
Yang, C. et al. Fecal IgA levels are determined by strain-level differences in bacteroides ovatus and are modifiable by gut microbiota manipulation. Cell Host Microbe 27, 467â475.e6 (2020).
Spindler, M. P. et al. Human gut microbiota stimulate defined innate immune responses that vary from phylum to strain. Cell Host Microbe 30, 1481â1498.e5 (2022).
Zhao, S. et al. Adaptive evolution within gut microbiomes of healthy people. Cell Host Microbe 25, 656â667.e8 (2019).
Aggarwala, V. et al. Precise quantification of bacterial strains after fecal microbiota transplantation delineates long-term engraftment and explains outcomes. Nat. Microbiol. 6, 1309â1318 (2021).
Conwill, A. et al. Anatomy promotes neutral coexistence of strains in the human skin microbiome. Cell Host Microbe 30, 171â182.e7 (2022).
Olm, M. R. et al. inStrain profiles population microdiversity from metagenomic data and sensitively detects shared microbial strains. Nat. Biotechnol. 39, 727â736 (2021).
Drewes, J. L. et al. Transmission and clearance of potential procarcinogenic bacteria during fecal microbiota transplantation for recurrent Clostridioides difficile. JCI Insight 4, 130848 (2019).
Vatanen, T. et al. Genomic variation and strain-specific functional adaptation in the human gut microbiome during early life. Nat. Microbiol. 4, 470â479 (2019).
Zheng, W. et al. High-throughput, single-microbe genomics with strain resolution, applied to a human gut microbiome. Science 376, eabm1483 (2022).
Gupta, S. et al. LB973 Cutaneous surgical wounds have distinct microbiomes from intact skin. J. Invest. Dermatol. 142, B24 (2022).
Truong, D. T., Tett, A., Pasolli, E., Huttenhower, C. & Segata, N. Microbial strain-level population structure and genetic diversity from metagenomes. Genome Res. 27, 626â638 (2017).
Yatsunenko, T. et al. Human gut microbiome viewed across age and geography. Nature 486, 222â227 (2012).
Valles-Colomer, M. et al. The person-to-person transmission landscape of the gut and oral microbiomes. Nature 614, 125â135 (2023).
Schmidt, T. S. B. et al. Drivers and determinants of strain dynamics following fecal microbiota transplantation. Nat. Med. 28, 1902â1912 (2022).
Schloss, P. D., Iverson, K. D., Petrosino, J. F. & Schloss, S. J. The dynamics of a familyâs gut microbiota reveal variations on a theme. Microbiome 2, 25 (2014).
Tamburini, F. B. et al. Precision identification of diverse bloodstream pathogens in the gut microbiome. Nat. Med. 24, 1809â1814 (2018).
Dsouza, M. et al. Colonization of the live biotherapeutic product VE303 and modulation of the microbiota and metabolites in healthy volunteers. Cell Host Microbe 30, 583â598.e8 (2022).
Siranosian, B. A. et al. Rare transmission of commensal and pathogenic bacteria in the gut microbiome of hospitalized adults. Nat. Commun. 13, 586 (2022).
Garud, N. R., Good, B. H., Hallatschek, O. & Pollard, K. S. Evolutionary dynamics of bacteria in the gut microbiome within and across hosts. PLoS Biol. 17, e3000102 (2019).
Blaser, M. J. Missing Microbes: How the Overuse of Antibiotics Is Fueling Our Modern Plagues (Henry Holt and Co., 2014).
Ni, J., Wu, G. D., Albenberg, L. & Tomov, V. T. Gut microbiota and IBD: causation or correlation? Nat. Rev. Gastroenterol. Hepatol. 14, 573â584 (2017).
Raffals, L. E. et al. The development and initial findings of a study of a prospective adult research cohort with inflammatory bowel disease (SPARC IBD). Inflamm. Bowel Dis. 28, 192â199 (2022).
Schnorr, S. L. et al. Gut microbiome of the Hadza hunter-gatherers. Nat. Commun. 5, 3654 (2014).
Yassour, M. et al. Natural history of the infant gut microbiome and impact of antibiotic treatment on bacterial strain diversity and stability. Sci. Transl. Med. 8, 343ra81 (2016).
Lee, S. M. et al. Bacterial colonization factors control specificity and stability of the gut microbiota. Nature 501, 426â431 (2013).
Verster, A. J. et al. The landscape of type VI secretion across human gut microbiomes reveals its role in community composition. Cell Host Microbe 22, 411â419.e4 (2017).
Han, S. R. et al. Helicobacter pylori: clonal population structure and restricted transmission within families revealed by molecular typing. J. Clin. Microbiol. 38, 3646â3651 (2000).
Saheb Kashaf, S. et al. Staphylococcal diversity in atopic dermatitis from an individual to a global scale. Cell Host Microbe 31, 578â592.e6 (2023).
Paramsothy, S. et al. Multidonor intensive faecal microbiota transplantation for active ulcerative colitis: a randomised placebo-controlled trial. Lancet 389, 1218â1228 (2017).
Faith, J. J. et al. The long-term stability of the human gut microbiota. Science 341, 1237439 (2013).
Faith, J. J., Colombel, J.-F. & Gordon, J. I. Identifying strains that contribute to complex diseases through the study of microbial inheritance. Proc. Natl Acad. Sci. USA 112, 633â640 (2015).
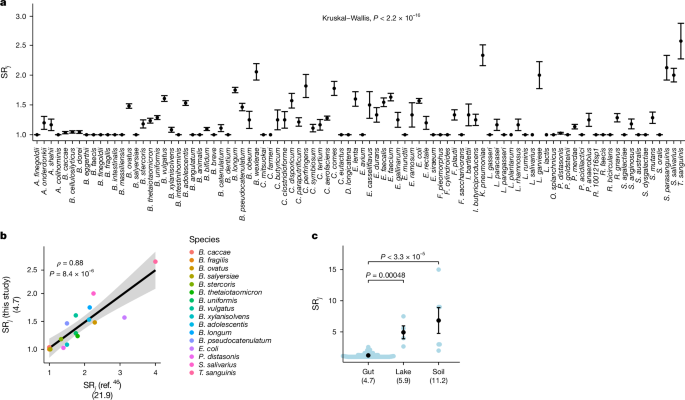
Faith, J. J. et al. Strain population structure varies widely across bacterial species and predicts strain colonization in unrelated individuals. Preprint at bioRxiv https://doi.org/10.1101/2020.10.17.343640 (2020).
Jain, C., Rodriguez-R, L. M., Phillippy, A. M., Konstantinidis, K. T. & Aluru, S. High throughput ANI analysis of 90K prokaryotic genomes reveals clear species boundaries. Nat. Commun. 9, 5114 (2018).
Rodriguez-R, L. M. et al. An ANI gap within bacterial species that advances the definitions of intra-species units. mBio 15, e02696-23 (2024).
Seekatz, A. M., Rao, K., Santhosh, K. & Young, V. B. Dynamics of the fecal microbiome in patients with recurrent and nonrecurrent Clostridium difficile infection. Genome Med. 8, 47 (2016).
Contijoch, E. J. et al. Gut microbiota density influences host physiology and is shaped by host and microbial factors. eLife 8, e40553 (2019).
Weingarden, A. et al. Dynamic changes in short- and long-term bacterial composition following fecal microbiota transplantation for recurrent Clostridium difficile infection. Microbiome 3, 10 (2015).
Faith, J. J., McNulty, N. P., Rey, F. E. & Gordon, J. I. Predicting a human gut microbiotaâs response to diet in gnotobiotic mice. Science 333, 101â104 (2011).
Bahtiyar Yilmaz, A. et al. Long-term evolution and short-term adaptation of microbiota strains and sub-strains in mice. Cell Host Microbe 29, 650â663.e9 (2021).
McNulty, N. P. et al. Effects of diet on resource utilization by a model human gut microbiota containing Bacteroides cellulosilyticus WH2, a symbiont with an extensive glycobiome. PLoS Biol. 11, e1001637 (2013).
Walker, A. W. et al. Dominant and diet-responsive groups of bacteria within the human colonic microbiota. ISME J 5, 220â230 (2011).
Poyet, M. et al. A library of human gut bacterial isolates paired with longitudinal multiomics data enables mechanistic microbiome research. Nat. Med. 25, 1442â1452 (2019).
Seemann, T. Prokka: rapid prokaryotic genome annotation. Bioinformatics 30, 2068â2069 (2014).
Page, A. J. et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics 31, 3691â3693 (2015).
Brynildsrud, O., Bohlin, J., Scheffer, L. & Eldholm, V. Rapid scoring of genes in microbial pan-genome-wide association studies with Scoary. Genome Biol 17, 238 (2016).
Hernández-Plaza, A. et al. eggNOG 6.0: enabling comparative genomics across 12 535 organisms. Nucleic Acids Res. 51, D389âD394 (2023).
Forbes, J. D. et al. A comparative study of the gut microbiota in immune-mediated inflammatory diseasesâdoes a common dysbiosis exist? Microbiome 6, 221 (2018).
Pascal, V. et al. A microbial signature for Crohnâs disease. Gut 66, 813â822 (2017).
Michail, S. et al. Alterations in the gut microbiome of children with severe ulcerative colitis. Inflamm. Bowel Dis. 18, 1799â1808 (2012).
Antharam, V. C. et al. Intestinal dysbiosis and depletion of butyrogenic bacteria in Clostridium difficile infection and nosocomial diarrhea. J. Clin. Microbiol. 51, 2884â2892 (2013).
Hirten, R. P. et al. Microbial engraftment and efficacy of fecal microbiota transplant for Clostridium difficile in patients with and without inflammatory bowel disease. Inflamm. Bowel Dis. 25, 969â979 (2019).
Terveer, E. M. et al. Faecal microbiota transplantation for Clostridioides difficile infection: four yearsâ experience of the Netherlands Donor Feces Bank. United Eur. Gastroenterol. J. 8, 1236â1247 (2020).
Ianiro, G. et al. Variability of strain engraftment and predictability of microbiome composition after fecal microbiota transplantation across different diseases. Nat. Med. 28, 1913â1923 (2022).
Smith, V. H. Microbial diversity-productivity relationships in aquatic ecosystems. FEMS Microbiol. Ecol. 62, 181â186 (2007).
Graham, J. H. & Duda, J. J. The humpbacked species richness-curve: a contingent rule for community ecology. Int. J. Ecol. 2011, e868426 (2011).
Sassone-Corsi, M. et al. Microcins mediate competition among Enterobacteriaceae in the inflamed gut. Nature 540, 280â283 (2016).
Becattini, S. et al. Commensal microbes provide first line defense against Listeria monocytogenes infection. J. Exp. Med. 214, 1973â1989 (2017).
Caballero, S. et al. Cooperating commensals restore colonization resistance to vancomycin-resistant Enterococcus faecium. Cell Host Microbe 21, 592â602.e4 (2017).
Ducarmon, Q. R. et al. Gut microbiota and colonization resistance against bacterial enteric infection. Microbiol Mol Biol Rev 83, e00007âe00019 (2019).
Donia, M. S. et al. A systematic analysis of biosynthetic gene clusters in the human microbiome reveals a common family of antibiotics. Cell 158, 1402â1414 (2014).
Chatzidaki-Livanis, M., Coyne, M. J. & Comstock, L. E. An antimicrobial protein of the gut symbiont Bacteroides fragilis with a MACPF domain of host immune proteins. Mol. Microbiol. 94, 1361â1374 (2014).
Roelofs, K. G., Coyne, M. J., Gentyala, R. R., Chatzidaki-Livanis, M. & Comstock, L. E. Bacteroidales secreted antimicrobial proteins target surface molecules necessary for gut colonization and mediate competition in vivo. mBio 7, e01055â16 (2016).
Cohan, F. M. Transmission in the origins of bacterial diversity, from ecotypes to phyla. Microbiol. Spectr. https://doi.org/10.1128/microbiolspec.mtbp-0014-2016 (2017).
Leslie, J. L. et al. Protection from lethal Clostridioides difficile infection via intraspecies competition for cogerminant. mBio 12, e00522â21 (2021).
Fung, C. et al. High-resolution mapping reveals that microniches in the gastric glands control Helicobacter pylori colonization of the stomach. PLoS Biol. 17, e3000231 (2019).
Balato, A. et al. Human microbiome: composition and role in inflammatory skin diseases. Arch. Immunol. Ther. Exp. (Warsz.). 67, 1â18 (2019).
Browne, H. P. et al. Culturing of âunculturableâ human microbiota reveals novel taxa and extensive sporulation. Nature 533, 543â546 (2016).
Lagier, J. C. et al. Culturing the human microbiota and culturomics. Nat. Rev. Microbiol. 16, 540â550 (2018).
De Filippis, F. et al. Distinct genetic and functional traits of human intestinal Prevotella copri strains are associated with different habitual diets. Cell Host Microbe 25, 444â453.e3 (2019).
Scher, J. U. et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. eLife 2, e01202 (2013).
Fehlner-Peach, H. et al. Distinct polysaccharide utilization profiles of human intestinal Prevotella copri isolates. Cell Host Microbe 26, 680â690.e5 (2019).
Lopez-Siles, M. et al. Alterations in the abundance and co-occurrence of Akkermansia muciniphila and Faecalibacterium prausnitzii in the colonic mucosa of inflammatory bowel disease subjects. Front. Cell. Infect. Microbiol. 8, 281 (2018).
Louie, T. et al. VE303, a defined bacterial consortium, for prevention of recurrent clostridioides difficile infection: a randomized clinical trial. JAMA 329, 1356â1366 (2023).
Nooij, S. et al. Fecal microbiota transplantation influences procarcinogenic Escherichia coli in recipient recurrent Clostridioides difficile patients. Gastroenterology 161, 1218â1228.e5 (2021).
Nooij, S. et al. Long-term beneficial effect of faecal microbiota transplantation on colonisation of multidrug-resistant bacteria and resistome abundance in patients with recurrent Clostridioides difficile infection. Genome Med. 16, 37 (2024).
Britton, G. J. et al. Microbiotas from humans with inflammatory bowel disease alter the balance of gut Th17 and RORγt+ regulatory T cells and exacerbate colitis in mice. Immunity 50, 212â224 (2019).
Gurevich, A., Saveliev, V., Vyahhi, N. & Tesler, G. QUAST: quality assessment tool for genome assemblies. Bioinformatics 29, 1072â1075 (2013).
Llewellyn, S. R. et al. Interactions between diet and the intestinal microbiota alter intestinal permeability and colitis severity in mice. Gastroenterology 154, 1037â1046.e2 (2018).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Methodol. 57, 289â300 (1995).
Chen-Liaw, A. Source Data. Zenodo https://doi.org/10.5281/zenodo.13942097 (2024).