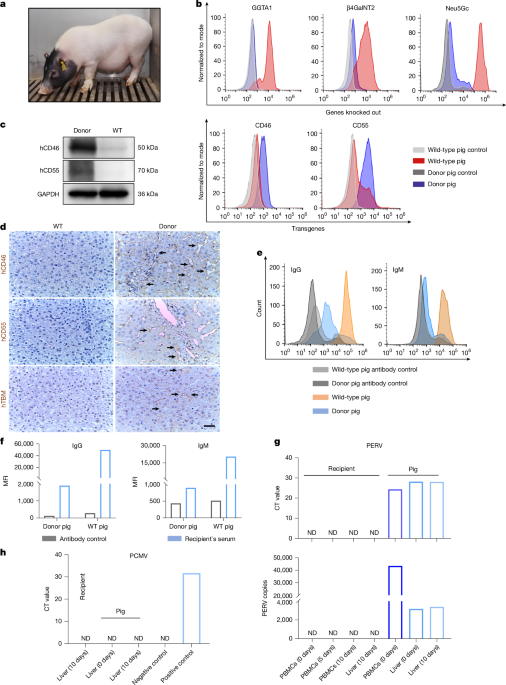
Xenotransplantation has entered the era of clinical research. Research teams at the University of Maryland School of Medicine have performed pig-to-human heart transplantation and scientists at both Massachusetts General Hospital and New York University recently carried out pig-to-human kidney transplantation3,4,5,6,7. Scientists from the University of Pennsylvania used a porcine liver to treat a brain-dead person with liver failure12. The current study was performed to preliminarily evaluate the feasibility of pig-to-human liver xenotransplantation. The use of genetic modification and a designated pathogen-free environment may have prevented hyperacute rejection and potential PERV, PCMV or other porcine virus infections in the recipient.
As described, a heterotopic auxiliary liver transplantation was performed. To ensure the best match, the calibre and flow velocity of main blood vessels in the donor and recipient were assessed before surgery. This guaranteed sufficient blood perfusion in the xenograft and hemodynamic stability in the recipient, avoiding graft dysfunction caused by haemodynamic disorders, as reported in ref. 6. Auxiliary liver transplantation is an ideal bridge therapy for individuals with liver failure, because it is not difficult to remove pig liver and reconstruct the IVC when the function of the original liver is restored or when a suitable donor liver is available. We removed the xenograft and reconstructed the IVC at the end of the study to simulate the abovementioned situation. Moreover, our heterotopic auxiliary liver transplantation protocol improved the efficiency of interventional thrombolysis directly from the deep vein of the lower limb. The first case of pig-to-human heart xenotransplantation found microthrombi in the terminal stage biopsies7. Similarly, the current study found that D-dimer levels were transiently elevated shortly after surgery (Extended Data Fig. 5a). Timely thrombolysis was then used to keep the xenograft functional.
Indeed, the flow in the infrarenal IVC is not physiological. To achieve physiological haemodynamics, we must perform auxiliary partial orthotopic liver transplantation. However, this will remove part of the original liver and may cause potential complications such as liver malfunction, bile leakage or bleeding in patients. Because our goal is to assist patients with acute liver failure through the critical period, there is no need to perform a transplantation that fully conforms to physiology. As long as the xenograft can provide metabolic and coagulation functions for a certain time, this transplantation is sufficient. In this study, we used the blood flow of the IVC to supply the xenograft, which then successfully returned to the heart. Throughout the whole study, no oedema was observed in the lower limbs, indicating that the lower limb circulation was guaranteed. More importantly, the xenograft remained functional and the haemodynamics remained stable until study completion. Therefore, non-physiological flow in this study did not cause severe disturbance.
Hyperacute rejection is one of the most critical issues with xenotransplantation in preclinical models18. Fortunately, no evidence of hyperacute rejection was found in the current study. In addition to editing the glycoprotein α-galactosyltransferase 1 gene, a series of immunosuppressive agents were used, of which tacrolimus (FK506) played a vital role. During the early stage of this xenotransplantation, we used tacrolimus at a concentration of 5 mg l−1 (the upper limit of normal), according to our previous protocol. However, a high blood concentration of tacrolimus was noted at postoperative day 2, which might result from the heterogeneity of drug metabolism. We adjusted the dose in time. At the late stage of this experiment, the level of total bilirubin was elevated, which may be related to the toxicity of tacrolimus.
Whether to use Rituxan (rituximab) during induction immunosuppression was one of the focuses of our pre-operative discussion. Because of the huge advantages of gene editing, humoral immunity no longer has a major impact on graft survival. Therefore, Rituxan was not included in the immunosuppression strategy of works related to liver xenotransplantation19,20. Similarly, we did not use Rituxan in our previous trails of pig-to-monkey xenotransplantation, because B cells were not activated in these studies13. Therefore, in this study, Rituxan was not used initially. When B cells started to be augmented, we had to adopt Rituxan, along with plasma exchange and intravenous immunoglobulin therapy, which theoretically can remove the formed antibodies and plasmacytes. This trial indicates that the activation of B cells might occur in pig-to-human liver xenotransplantation. Further investigation is needed before we can incorporate Rituxan into our induction immunosuppressive strategy.
The discrepancy in ALT and AST amounts was unexpected and something that has not been observed in previous animal studies. More interestingly, a spike in AST during the early stage was detected in a pig-to-human heart xenotransplantation performed in a previous study6. It is plausible that AST was released by myocardial cells. This is supported by the early increase in creatine kinase and creatinine kinase-myocardial band amounts observed at the same time point (Extended Data Fig. 7e). Consequently, myocardial damage should be assessed at the early stage of liver transplantation and pharmacological myocardial protection implemented if necessary. Notably, some cholestasis was observed in the recipient’s original liver tissue on day 10, which may explain the elevated bilirubin observed later. However, this was absent in the xenograft. Thus, it is probable that current therapeutic drugs are slightly less toxic to pig liver than to human liver.
Abnormity in coagulation is a main cause of xenograft dysfunction21, and occurred in the first pig-to-human cardiac xenotransplantation7 and in our previous cases of pig-to-monkey liver xenotransplantation. However, no serious bleeding or clotting disorder occurred in the current case. PT remained relatively stable after surgery, APTT increased transiently at the early stage and later declined, and PLT decreased transiently in the early stage and later increased. Bleeding disorders and coagulopathies were considerably milder in this brain-dead recipient than in previous monkey recipients, indicating that humanized genetic modifications may function better in humans. Because of the advantages of heterotopic auxiliary liver transplantation, we were able to intervene after the early elevation of D-dimer and prevent potential PV thrombosis.
Future studies will need to choose between a bridge graft or permanent placement of xenotransplantation. Although the xenograft could secrete bile and produce porcine albumin in this study, it is unlikely that the production of bile and porcine albumin was enough to support the human body for a long period. Consequently, as indicated in ref. 17, current liver xenotransplantation modalities may be more suitable as an adjuvant bridge therapy for individuals with liver failure who are waiting for a human liver. Nevertheless, it will be important to design effective orthotopic pig-to-human liver xenotransplantation methods for future patients.
We admit the limitations of this study. First, at the request of the recipient’s family members, the study was terminated on day 10, which made the follow-up period insufficient to analyse alterations in xenograft function over a long period. Second, at present, we could measure only the basic functions of the liver, such as the synthesis of albumin and the secretion of bile. However, this unique pig-to-human liver xenotransplantation can still provide critical information that cannot be provided by animal experiments alone.