Silver, J. & Miller, J. H. Regeneration beyond the glial scar. Nat. Rev. Neurosci. 5, 146â156 (2004).
Tran, A. P., Warren, P. M. & Silver, J. New insights into glial scar formation after spinal cord injury. Cell Tissue Res. 387, 319â336 (2021).
Johansson, C. B. et al. Identification of a neural stem cell in the adult mammalian central nervous system. Cell 96, 25â34 (1999).
Meletis, K. et al. Spinal cord injury reveals multilineage differentiation of ependymal cells. PLoS Biol. 6, e182 (2008).
Sabelström, H. et al. Resident neural stem cells restrict tissue damage and neuronal loss after spinal cord injury in mice. Science 342, 637â640 (2013).
Barnabé-Heider, F. et al. Origin of new glial cells in intact and injured adult spinal cord. Cell Stem Cell 7, 470â482 (2010).
Lacroix, S. et al. Central canal ependymal cells proliferate extensively in response to traumatic spinal cord injury but not demyelinating lesions. PLoS ONE 9, e85916 (2014).
New, L. E., Yanagawa, Y., McConkey, G. A., Deuchars, J. & Deuchars, S. A. GABAergic regulation of cell proliferation within the adult mouse spinal cord. Neuropharmacology 223, 109326 (2023).
Vigh, B., Vigh-Teichmann, I., Manzano e Silva, M. J. & van den Pol, A. N. Cerebrospinal fluid-contacting neurons of the central canal and terminal ventricle in various vertebrates. Cell Tissue Res. 231, 615â621 (1983).
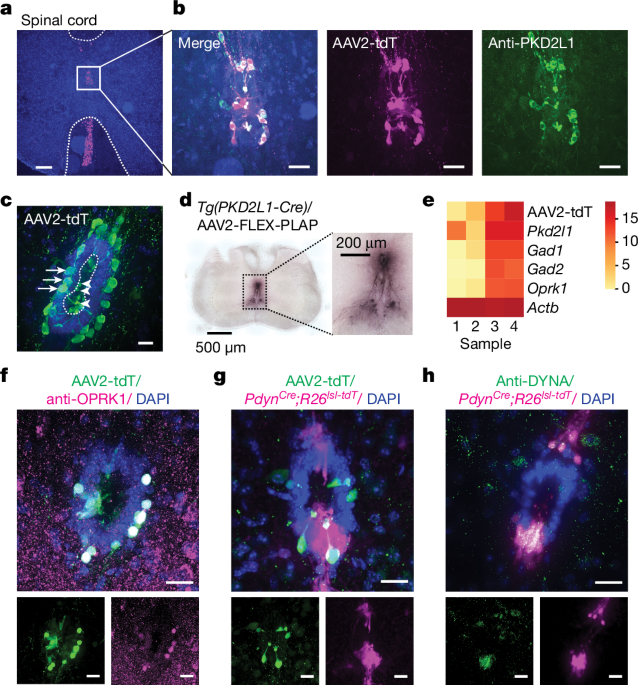
Huang, A. L. et al. The cells and logic for mammalian sour taste detection. Nature 442, 934â938 (2006).
Orts-Delâimmagine, A. et al. Properties of subependymal cerebrospinal fluid contacting neurones in the dorsal vagal complex of the mouse brainstem. J. Physiol. 590, 3719â3741 (2012).
Prendergast, A. E. et al. CSF-contacting neurons respond to Streptococcus pneumoniae and promote host survival during central nervous system infection. Curr. Biol. https://doi.org/10.1016/J.CUB.2023.01.039 (2023).
Böhm, U. L. et al. CSF-contacting neurons regulate locomotion by relaying mechanical stimuli to spinal circuits. Nat. Commun. 7, 10866 (2016).
Sternberg, J. R. et al. Pkd2l1 is required for mechanoception in cerebrospinal fluid-contacting neurons and maintenance of spine curvature. Nat. Commun. 9, 3804 (2018).
Orts-DelâImmagine, A. et al. A single polycystic kidney disease 2-like 1 channel opening acts as a spike generator in cerebrospinal fluid-contacting neurons of adult mouse brainstem. Neuropharmacology 101, 549â565 (2016).
Johnson, E. et al. Graded spikes differentially signal neurotransmitter input in cerebrospinal fluid contacting neurons of the mouse spinal cord. iScience 26, 105914 (2023).
Gerstmann, K. et al. The role of intraspinal sensory neurons in the control of quadrupedal locomotion. Curr. Biol. 32, 2442â2453.e4 (2022).
Djenoune, L. et al. The dual developmental origin of spinal cerebrospinal fluid-contacting neurons gives rise to distinct functional subtypes. Sci Rep. 7, 719 (2017).
Nakamura, Y. et al. Cerebrospinal fluid-contacting neuron tracing reveals structural and functional connectivity for locomotion in the mouse spinal cord. eLife 12, e83108 (2023).
Stoeckel, M.-E. et al. Cerebrospinal fluid-contacting neurons in the rat spinal cord, a γ-aminobutyric acidergic system expressing the P2X2 subunit of purinergic receptors, PSA-NCAM, and GAP-43 immunoreactivities: light and electron microscopic study. J. Comp. Neurol. 457, 159â174 (2003).
Chavkin, C. Dynorphin â still an extraordinarily potent opioid peptide. Mol. Pharmacol. 83, 729â736 (2013).
Khachaturian, H. et al. Dynorphin immunocytochemistry in the rat central nervous system. Peptides 3, 941â954 (1982).
Veldman, M. B. et al. Brainwide genetic sparse cell labeling to illuminate the morphology of neurons and glia with Cre-dependent MORF mice. Neuron 108, 111â127.e6 (2020).
Furube, E. et al. Neural stem cell phenotype of tanycyte-like ependymal cells in the circumventricular organs and central canal of adult mouse brain. Sci. Rep. 10, 2826 (2020).
Brust, T. F. Biased ligands at the κ opioid receptor: fine-tuning receptor pharmacology. Handb. Exp. Pharmacol. 271, 115â135 (2022).
Bruchas, M. R. & Chavkin, C. Kinase cascades and ligand-directed signaling at the κ opioid receptor. Psychopharmacology 210, 137â147 (2010).
Eriksson, P. S., Nilsson, M., WÃ¥gberg, M., Hansson, E. & Rönnbäck, L. κ-Opioid receptors on astrocytes stimulate l-type Ca2+ channels. Neuroscience 54, 401â407 (1993).
Gurwell, J. A. et al. κ-Opioid receptor expression defines a phenotypically distinct subpopulation of astroglia: relationship to Ca2+ mobilization, development, and the antiproliferative effect of opioids. Brain Res. 737, 175â187 (1996).
Pan, Z. Z. Opioid receptor-mediated enhancement of the hyperpolarization-activated current (Ih) through mobilization of intracellular calcium in rat nucleus raphe magnus. J. Physiol. 548, 765â775 (2003).
Lai, J. et al. Dynorphin A activates bradykinin receptors to maintain neuropathic pain. Nat. Neurosci. 9, 1534â1540 (2006).
Laughlin, T. M. et al. Spinally administered dynorphin A produces long-lasting allodynia: involvement of NMDA but not opioid receptors. Pain 72, 253â260 (1997).
Bakshi, R. & Faden, A. I. Competitive and non-competitive NMDA antagonists limit dynorphin A-induced rat hindlimb paralysis. Brain Res. 507, 1â5 (1990).
Zhang, S. et al. Dynorphin A as a potential endogenous ligand for four members of the opioid receptor gene family. J. Pharmacol. Exp. Ther. 286, 136â141 (1998).
Riondel, P. et al. Evidence for two subpopulations of cerebrospinal-fluid contacting neurons with opposite GABAergic signaling in adult mouse spinal cord. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.2289-22.2024 (2024).
Corns, L. F. et al. Cholinergic enhancement of cell proliferation in the postnatal neurogenic niche of the mammalian spinal cord. Stem Cells 33, 2864â2876 (2015).
Hussein, S. A. Functional characterization of the TRP-type channel PKD2L1. ERA https://doi.org/10.7939/R3P84495F (2015).
Felix, R. Molecular regulation of voltage-gated Ca2+ channels. J. Recept. Signal Transduct. 25, 57â71 (2008).
Barber, R. P., Vaughn, J. E. & Roberts, E. The cytoarchitecture of GABAergic neurons in rat spinal cord. Brain Res. 238, 305â328 (1982).
Djenoune, L. et al. Investigation of spinal cerebrospinal fluid-contacting neurons expressing PKD2L1: evidence for a conserved system from fish to primates. Front. Neuroanat. 8, 26 (2014).
Matson, K. J. E. et al. Single cell atlas of spinal cord injury in mice reveals a pro-regenerative signature in spinocerebellar neurons. Nat. Commun. 13, 5628 (2022).
Ren, Y. et al. Ependymal cell contribution to scar formation after spinal cord injury is minimal, local and dependent on direct ependymal injury. Sci Rep. 7, 41122 (2017).
Corns, L. F., Deuchars, J. & Deuchars, S. A. GABAergic responses of mammalian ependymal cells in the central canal neurogenic niche of the postnatal spinal cord. Neurosci. Lett. 553, 57â62 (2013).
Kozono, H., Yoshitani, H. & Nakano, R. Post-marketing surveillance study of the safety and efficacy of nalfurafine hydrochloride (Remitch® capsules 2.5âμg) in 3,762 hemodialysis patients with intractable pruritus. Int. J. Nephrol. Renovasc. Dis. 11, 9â24 (2018).
Bloodgood, D. W. et al. κ Opioid receptor and dynorphin signaling in the central amygdala regulates alcohol intake. Mol. Psychiatry 26, 2187â2199 (2021).
Madisen, L. et al. A robust and high-throughput Cre reporting and characterization system for the whole mouse brain. Nat. Neurosci. 13, 133â140 (2010).
Krashes, M. J. et al. An excitatory paraventricular nucleus to AgRP neuron circuit that drives hunger. Nature 507, 238â242 (2014).
Gee, J. M. et al. Imaging activity in neurons and glia with a Polr2a-based and Cre-dependent GCaMP5G-IRES-tdTomato reporter mouse. Neuron 83, 1058â1072 (2014).
Buch, T. et al. A Cre-inducible diphtheria toxin receptor mediates cell lineage ablation after toxin administration. Nat. Methods 2, 419â426 (2005).
Arnold, K. et al. Sox2+ adult stem and progenitor cells are important for tissue regeneration and survival of mice. Cell Stem Cell 9, 317â329 (2011).
Edelstein, A. D. et al. Advanced methods of microscope control using μManager software. J. Biol. Methods 1, e10 (2014).
Renier, N. et al. iDISCO: a simple, rapid method to immunolabel large tissue samples for volume imaging. Cell 159, 896â910 (2014).