Every day around mid-morning, Joan retreats into the bedroom of her central Massachusetts home. She lowers the window blinds, settles into her favourite armchair and puts on a special headset.
For an hour, she surrenders to an immersive audiovisual experience of rhythmic clicking and flashing lights — tuned to repeat 40 times a second. Designed to synchronize particular electrical patterns called gamma waves in her brain, the sound-and-light show aims to combat the effects of dementia. “It’s relaxing, in a way,” says Joan, 78, who was diagnosed with early-stage Alzheimer’s disease two years ago. “I just kind of sit there.”
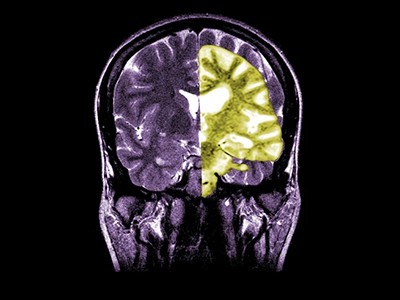
After a year of this routine, scans taken in mid-June showed that Joan’s brain volume had remained stable. Memory tests found that her cognitive decline had stopped as well.
Anecdotes such as Joan’s might seem hard to believe — and neuroscientist Li-Huei Tsai is no stranger to such scepticism. She and her colleagues at the Massachusetts Institute of Technology (MIT) in Cambridge first reported1 that flickering lights had beneficial effects on mice with Alzheimer’s-like conditions in 2016.
Many researchers dismissed the results. “A lot of people just said, ‘This is too good to be true. This cannot be real,’” Tsai says. To prove her critics wrong, she realized she needed human data. So, Tsai — along with her MIT collaborator, synthetic neurobiologist Ed Boyden — co-founded a company called Cognito Therapeutics (also based in Cambridge). Within two years, they initiated clinical trials, and have since tested the technology on hundreds of individuals.
Humanity’s newest brain gains are most at risk from ageing
So far, the results have provided encouraging evidence of neuroprotection, with none of the serious side effects, such as brain swelling or bleeding, that often accompany the antibody drugs currently available or nearing regulatory approval for Alzheimer’s disease. “Everything is going in the right direction,” says Allan Levey, a neurologist at Emory University School of Medicine in Atlanta, Georgia, and an adviser to Cognito.
Nevertheless, Levey has worked in the field for long enough to know that the vast majority of promising therapies for Alzheimer’s eventually end up in the dustbin of drug-development history, with more than 98% of all mid- to late-stage clinical trials ending in failure. And, although research from the MIT team and others continues to build a solid scientific foundation for this unconventional strategy, some groups have not managed to replicate their findings in mice.
Now, all eyes are trained on a large, randomized trial involving more than 600 participants, including Joan. “I feel optimistic, but I also like to be cautious,” says Fiza Singh, a psychiatrist at the University of California, San Diego. “When you have a convergence of data like that, it says to me that there is some signal — something is going on.”
Many, however, are not waiting for further validation. A cottage industry has already sprung up around devices marketed as ‘wellness’ products that put flashing lights and clicking sounds into desk lamps or smartphone apps, all claiming to improve brain health. This has sparked concern among some researchers that the rush to market might be getting ahead of the science, which could harm consumers.
Yet, as the buzz surrounding this treatment grows, so does the pressure to separate hype from reality. The challenge for scientists is to confirm whether the approach offers more than just flickers of hope.
Guided by gamma
Alzheimer’s disease is characterized mainly by the accumulation of amyloid-β plaques and tau tangles in the brain. These protein structures are thought to interfere with neuronal communication and result in cell death. However, in the early 1990s, neuroscientist Rodolfo Llinás and his colleagues at New York University (NYU) Medical Center noticed another intriguing hallmark of the disease.
While studying the magnetic fields produced by neuronal activity, they discovered a deficiency in some of the brain’s fastest-firing waves — specifically, those in the gamma frequency band, which oscillate at around 40 hertz. In individuals with Alzheimer’s disease, these gamma waves, which are crucial for processes such as attention and memory, were weaker than those of cognitively healthy individuals2.

Cognito’s prototype device is in testing.Credit: David L. Ryan/The Boston Globe via Getty
Over the years, other groups have made similar, corroborating observations. However, it was not until 2016, through the work of Tsai and Boyden, that a viable strategy emerged to address — and reverse — this gamma deficiency.
The MIT researchers initially induced gamma waves in mouse brains using a complex technique that involved genetically modifying neurons and then implanting optical fibres through the skull1. They then developed less invasive methods, such as simple strip lights, mini sound systems or vibrating subwoofers near the animals’ cages.
The rhythmic cues engage the brain through what Ralph Kern, Cognito’s chief medical officer, describes as “sensory on-ramps” — areas in the cortex responsible for processing sensory information. From there, the gamma signal spreads to deeper brain regions, such as the hypothalamus, that play key parts in memory and cognition.
With repeated exposure comes brain ‘entrainment’: the firing patterns of neurons start to align with the rhythm of the stimulus. Synapses strengthen. Inflammation subsides. And, as the MIT team reported3 in February, 40-hertz stimulation also activates a neural-cleansing mechanism in mice, in which cerebrospinal fluid enters the brain, collects molecular debris and exits through specialized waste-removal channels. An independent team in China and Portugal has since replicated this finding4, and researchers at Boston University in Massachusetts have shown that the same process is activated by visual flickers in humans, as well5.
How menopause reshapes the brain
“There is a constellation of health-promoting effects,” Boyden says, and the results were consistent across several mouse models of Alzheimer’s. “That got me really excited about the translational possibilities,” he says.
Among all the documented effects of the treatment, “it’s not entirely clear which ones are crucial for therapeutic efficacy”, says neurobiologist Annabelle Singer, a former postdoctoral fellow in Boyden’s lab who contributed to many of the early studies and continues to investigate the phenomenon at the Georgia Institute of Technology in Atlanta. But Singer, a Cognito adviser, is confident about the overall impact. “We have widespread modulation of human circuits, including in cognitive regions,” she says. “And these circuits kind of kick into high gear in response to 40-hertz stimulation.”
On the same wavelength
The potential benefits are not limited to Alzheimer’s disease. Researchers have found positive effects of sensory stimulation in mouse models of autism spectrum disorder, stroke, multiple sclerosis and chemotherapy-related cognitive impairment. In humans, there is early evidence of favourable outcomes for children with insomnia and adults with treatment-resistant epilepsy (see, for example, ref. 6), with trials now ongoing for people with depression, Parkinson’s disease and head trauma.
Yet, despite the many mechanistic papers published by the MIT team and other scientists, not everyone is convinced that the therapy does what it says on the tin. Last year, two independent research groups — one led by neuroscientist György Buzsáki at NYU7, the other by neuroscientist Ted Weita Lai at China Medical University in Taichung, Taiwan8 — described their own investigations of flickering light therapy in mouse models of Alzheimer’s disease. Neither team found any reduction in amyloid-β levels.
Methodological differences between these studies and the original MIT report might explain the conflicting results, proponents of the technique contend. And, although the most outspoken champions of 40-hertz therapy have financial stakes in the approach, they point to confirmatory studies published by independent groups without industry ties as validation of the science (see, for example, ref. 9). Nevertheless, both Buzsáki and Lai have urged the scientific community to exercise caution when it comes to interpreting mouse findings and extrapolating them to human therapeutic strategies.

The EVY light from OptoCeutics hides it’s ‘flicker’ with pulses that alternate at different wavelengths.Credit: OptoCeutics
More difficult to argue with might be the encouraging early clinical-trial data, says Sheng-Tau Hou, a neurobiologist at the Southern University of Science and Technology in Shenzhen, China. “Despite the fact that we don’t understand the molecular nitty-gritty of the mechanisms, the impact is quite obvious now,” he says.
Academic studies10 by the teams at MIT and Emory, along with industry-sponsored trials by Cognito researchers, have collectively found that 1–6 months of 40-hertz stimulation with both light and sound, delivered at home for an hour a day, can boost cognition, preserve brain volume, improve sleep quality, enhance the ability to do everyday tasks and induce favourable changes in brain immunity.
In one of the longest studies of its kind, Diane Chan, a neurologist at Massachusetts General Hospital in Boston and a postdoc in Tsai’s lab, is monitoring a handful of people with mild Alzheimer’s disease who have undergone daily 40-hertz treatment for 30 months and counting. Participants engage with the therapy through an easel-mounted light panel and soundbar system, with a tablet positioned in the centre so that users can entertain themselves with videos during each session.
Typically, individuals with early-stage Alzheimer’s disease perform progressively worse on standard neuropsychological tests, losing a few points every year. But in Chan’s study, participants’ test scores have remained stable. Brain volumes have shown no signs of shrinking and levels of a disease-associated protein in the blood have even trended downwards. “These patients have conquered the test of time,” says Chan, who presented the findings at an international conference on neurodegenerative diseases in March.
Debate rages over Alzheimer’s drug lecanemab as UK limits approval
At the same conference, Cognito reported similar benefits in both brain structure and cognitive function during 18 months of treatment with the company’s wearable technology — and some people have grown so attached to the daily routine of the sensory therapy that they have refused to return the device at the end of these studies, even though they are supposed to.
“Far be it from me to take this away from them,” says trial investigator Paul Solomon, a neuropsychologist who directs the Boston Center for Memory in Newton, Massachusetts, where Joan receives her treatment.
Roaring forty
For now, Cognito’s platform is accessible solely through clinical trials. However, some competing developers have already started marketing similar devices as holistic health aids, arguing that the technology is safe and that individuals can experience its potential cognitive benefits without the need for formal regulatory approval.
There are mobile-phone apps and websites that will make consumers’ devices flash and buzz at 40-hertz intervals. There are clicking-sound players, flickering light bulbs and stroboscopic desk lamps available for purchase online, ranging in price from US$50 to $274. And then there are more high-tech options, such as the ‘EVY Light’ from OptoCeutics, an academic spin-off firm with headquarters in Copenhagen and Berkeley, California. This shoebox-sized device delivers an ‘invisible spectral flicker’ — a white light created by two sets of light-emitting diodes, each emitting at different wavelengths and pulsing at 40 hertz but offset from one another.
The company’s founders have published evidence suggesting that the brain synchronizes its activity accordingly, even though the light appears steady11. The firm is now sponsoring a 62-person trial designed to test whether the device can help individuals with mild-to-moderate Alzheimer’s disease. However, with trial results and regulatory approvals potentially years away, OptoCeutics has elected to offer its light box to the public ahead of regulatory clearance. For $1,999, anyone can now have an EVY Light in their home.
“We want to be able to see how it can impact people now — today,” says co-founder and chief executive Mai Nguyen. “For us, the benefits outweigh the risks.”
Other 40-hertz technologies in development include a $1,799 headset by Vielight in Toronto, Canada, that administers near-infrared light through a series of strategically placed light-emitting diodes on the scalp, plus one clipped to a nostril and pointed up the nose. Pilot trials that included individuals with dementia have shown early signs of clinical potential.
Electrical-stimulation technologies can similarly provide targeted neuromodulation to specific brain areas with deficient gamma-wave activity. And in contrast to audiovisual approaches that administer 40-hertz stimuli — which remain inaccessible to people with hearing impairments, vision problems or other sensory-processing challenges — electrical stimulation should be broadly applicable, notes Barbara Borroni, a neurologist at the University of Brescia in Italy.
Several research groups are even combining 40-hertz stimulation with music therapy. In Japan, for example, a music technology company called VIE is integrating 40-hertz frequencies into ethereal music compositions designed to make the auditory stimuli more pleasing on the ear.
And at Northeastern University in Boston, music neuroscientist Psyche Loui and her colleagues are trialling a basketball-hoop-shaped device — developed by Oscillo Biosciences in Farmington, Connecticut, and nicknamed The Stargate — that synchronizes light with music, adding a rhythmic visual component tied to the beat of any song, while emitting a gentle flicker to promote brain activity in the gamma-frequency range.
The music, Loui says, makes the medicine go down easier: “People love the music. They tolerate the lights.”
A light touch
The lack of regulation and quality control worries some researchers, including Chan, who has done internal tests on several commercial devices and found that they often fail to consistently deliver 40-hertz flickers. She also warns that side effects such as headaches occur in an appreciable fraction of users. Moreover, for those prone to seizures, the flashing lights could pose serious risks.
“It’s really important to be a savvy consumer,” says Heather Snyder, head of medical and scientific operations at the Alzheimer’s Association, a non-profit research and advocacy organization in Chicago, Illinois.
Another concern is the potential for false hope and financial exploitation, particularly if company websites make outsized promises with their marketing materials. “It is definitely a grey area,” says Timothy Daly, a bioethicist and dementia researcher at the Bordeaux Population Health Research Centre in France. “It’s a very slippery slope — especially with the vulnerability of people who are worried about having Alzheimer’s.”
Conscious of those potential pitfalls, Cognito chief executive Christian Howell says the company has been “really purposeful about developing a very robust evidence base” for its device ahead of seeking marketing authorization, probably by early 2026. Alongside its year-long, randomized pivotal trial — which is on track to complete enrolment by the end of the year — Cognito is conducting an extension study, allowing participants such as Joan the opportunity to continue therapy for a further 12 months.
Joan didn’t hesitate to opt in. She and Art, her husband of 51 years, credit the Cognito device with stabilizing her condition, which remains manageable and allows Joan to maintain a high degree of functional independence. “It’s a godsend,” says Art. “If this froze everything the way it is right now, we could go to our graves living like this.”