Ciccarone, D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr. Opin. Psychiatry 34, 344–350 (2021).
Gamage, T. F. et al. Molecular and behavioral pharmacological characterization of abused synthetic cannabinoids MMB- and MDMB-FUBINACA, MN-18, NNEI, CUMYL-PICA, and 5-Fluoro-CUMYL-PICA. J. Pharmacol. Exp. Ther. 365, 437–446 (2018).
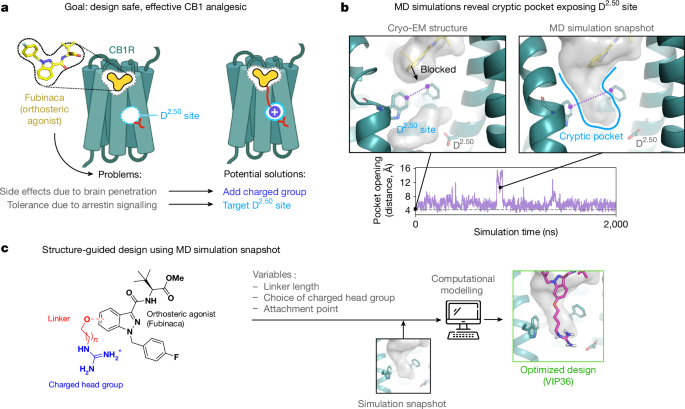
Zarzycka, B., Zaidi, S. A., Roth, B. L. & Katritch, V. Harnessing ion-binding sites for GPCR pharmacology. Pharmacol. Rev. 71, 571–595 (2019).
Nahin, R. L. Estimates of pain prevalence and severity in adults: United States, 2012. J. Pain 16, 769–780 (2015).
Cohen, S. P., Vase, L. & Hooten, W. M. Chronic pain: an update on burden, best practices, and new advances. Lancet 397, 2082–2097 (2021).
Volkow, N. D. & Blanco, C. The changing opioid crisis: development, challenges and opportunities. Mol. Psychiatry 26, 218–233 (2021).
Pertwee, R. G. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol. Ther. 74, 129–180 (1997).
Woodhams, S. G., Chapman, V., Finn, D. P., Hohmann, A. G. & Neugebauer, V. The cannabinoid system and pain. Neuropharmacology 124, 105–120 (2017).
Finlay, D. B. et al. Do toxic synthetic cannabinoid receptor agonists have signature in vitro activity profiles? A case study of AMB-FUBINACA. ACS Chem. Neurosci. 10, 4350–4360 (2019).
Banister, S. D. et al. Pharmacology of indole and indazole synthetic cannabinoid designer drugs AB-FUBINACA, ADB-FUBINACA, AB-PINACA, ADB-PINACA, 5F-AB-PINACA, 5F-ADB-PINACA, ADBICA, and 5F-ADBICA. ACS Chem. Neurosci. 6, 1546–1559 (2015).
Banister, S. D. et al. Pharmacology of valinate and tert-leucinate synthetic cannabinoids 5F-AMBICA, 5F-AMB, 5F-ADB, AMB-FUBINACA, MDMB-FUBINACA, MDMB-CHMICA, and their analogues. ACS Chem. Neurosci. 7, 1241–1254 (2016).
Wiley, J. L. et al. AB-CHMINACA, AB-PINACA, and FUBIMINA: affinity and potency of novel synthetic cannabinoids in producing Δ9-tetrahydrocannabinol-like effects in mice. J. Pharmacol. Exp. Ther. 354, 328–339 (2015).
Slivicki, R. A., Xu, Z., Mali, S. S. & Hohmann, A. G. Brain permeant and impermeant inhibitors of fatty-acid amide hydrolase suppress the development and maintenance of paclitaxel-induced neuropathic pain without producing tolerance or physical dependence in vivo and synergize with paclitaxel to reduce tumor cell line viability in vitro. Pharmacol. Res. 142, 267–282 (2019).
Henderson-Redmond, A. N. et al. c-Jun N terminal kinase signaling pathways mediate cannabinoid tolerance in an agonist-specific manner. Neuropharmacology 164, 107847 (2020).
Metna-Laurent, M., Mondésir, M., Grel, A., Vallée, M. & Piazza, P.-V. Cannabinoid-induced tetrad in mice. Curr. Protoc. Neurosci. 80, 9.59.1–9.59.10 (2017).
Clapper, J. R. et al. Anandamide suppresses pain initiation through a peripheral endocannabinoid mechanism. Nat. Neurosci. 13, 1265–1270 (2010).
Slivicki, R. A. et al. Brain-permeant and -impermeant inhibitors of fatty acid amide hydrolase synergize with the opioid analgesic morphine to suppress chemotherapy-induced neuropathic nociception without enhancing effects of morphine on gastrointestinal transit. J. Pharmacol. Exp. Ther. 367, 551–563 (2018).
Slivicki, R. A., Yi, J., Brings, V. E., Huynh, P. N. & Gereau, R. W. The cannabinoid agonist CB-13 produces peripherally mediated analgesia in mice but elicits tolerance and signs of central nervous system activity with repeated dosing. Pain 163, 1603–1621 (2022).
Gardin, A., Kucher, K., Kiese, B. & Appel-Dingemanse, S. Cannabinoid receptor agonist 13, a novel cannabinoid agonist: first in human pharmacokinetics and safety. Drug Metab. Dispos. 37, 827–833 (2009).
Ford, N. C. et al. Role of primary sensory neurone cannabinoid type-1 receptors in pain and the analgesic effects of the peripherally acting agonist CB-13 in mice. Br. J. Anaesth. 128, 159–173 (2022).
Seltzman, H. H. et al. Peripherally selective cannabinoid 1 receptor (CB1R) agonists for the treatment of neuropathic pain. J. Med. Chem. 59, 7525–7543 (2016).
Mulpuri, Y. et al. Synthetic peripherally-restricted cannabinoid suppresses chemotherapy-induced peripheral neuropathy pain symptoms by CB1 receptor activation. Neuropharmacology 139, 85–97 (2018).
Piscura, M. K. et al. Mechanisms of cannabinoid tolerance. Biochem. Pharmacol. 214, 115665 (2023).
Nguyen, P. T. et al. β-Arrestin2 regulates cannabinoid CB 1 receptor signaling and adaptation in a central nervous system region-dependent manner. Biol. Psychiatry 71, 714–724 (2012).
Ford, B. M. et al. Characterization of structurally novel G protein biased CB1 agonists: implications for drug development. Pharmacol. Res. 125, 161–177 (2017).
Liao, Y. Y. et al. Snapshot of the cannabinoid receptor 1-arrestin complex unravels the biased signaling mechanism. Cell 186, 5784–5797.e17 (2023).
Raehal, K. M. & Bohn, L. M. β-Arrestins: regulatory role and therapeutic potential in opioid and cannabinoid receptor-mediated analgesia. Handb. Exp. Pharmacol. 219, 427–443 (2014).
Breivogel, C. S., Lambert, J. M., Gerfin, S., Huffman, J. W. & Razdan, R. K. Sensitivity to Δ9-tetrahydrocannabinol is selectively enhanced in beta-arrestin2-/- mice. Behav. Pharmacol. 19, 298–307 (2008).
Wouters, E. et al. Assessment of biased agonism among distinct synthetic cannabinoid receptor agonist scaffolds. ACS Pharmacol. Transl. Sci. 3, 285–295 (2020).
Oleinikovas, V., Saladino, G., Cossins, B. P. & Gervasio, F. L. Understanding cryptic pocket formation in protein targets by enhanced sampling simulations. J. Am. Chem. Soc. 138, 14257–14263 (2016).
Wassman, C. D. et al. Computational identification of a transiently open L1/S3 pocket for reactivation of mutant p53. Nat. Commun. 4, 1407 (2013).
Ramos-Gonzalez, N., Paul, B. & Majumdar, S. IUPHAR themed review: opioid efficacy, bias, and selectivity. Pharmacol. Res. 197, 106961 (2023).
Manning, J. J., Rawcliffe, G., Finlay, D. B. & Glass, M. Cannabinoid 1 (CB1) receptor arrestin subtype-selectivity and phosphorylation dependence. Br. J. Pharmacol. 180, 369–382 (2023).
Faouzi, A. et al. Structure-based design of bitopic ligands for the µ-opioid receptor. Nature 613, 767–774 (2023).
Ople, R. S. et al. Signaling modulation mediated by ligand water interactions with the sodium site at μOR. ACS Cent. Sci. 10, 1490–1503 (2024).
Krishna Kumar, K. et al. Structure of a signaling cannabinoid receptor 1-G protein complex. Cell 176, 448–458.e12 (2019).
Krishna Kumar, K. et al. Structural basis for activation of CB1 by an endocannabinoid analog. Nat. Commun. 14, 2672 (2023).
Uprety, R. et al. Controlling opioid receptor functional selectivity by targeting distinct subpockets of the orthosteric site. eLife 10, 1–58 (2021).
Chakraborty, S. et al. A novel mitragynine analog with low-efficacy mu opioid receptor agonism displays antinociception with attenuated adverse effects. J. Med. Chem. 64, 13873–13892 (2021).
Qu, Q. et al. Insights into distinct signaling profiles of the µOR activated by diverse agonists. Nat. Chem. Biol. 19, 423–430 (2023).
Suomivuori, C.-M. et al. Molecular mechanism of biased signaling in a prototypical G protein-coupled receptor. Science 367, 881–887 (2020).
Wingler, L. M., McMahon, C., Staus, D. P., Lefkowitz, R. J. & Kruse, A. C. Distinctive activation mechanism for angiotensin receptor revealed by a synthetic nanobody. Cell 176, 479–490.e12 (2019).
Dziadulewicz, E. K. et al. Naphthalen-1-yl-(4-pentyloxynaphthalen-1-yl)methanone: a potent, orally bioavailable human CB1/CB2 dual agonist with antihyperalgesic properties and restricted central nervous system penetration. J. Med. Chem. 50, 3851–3856 (2007).
Lichtman, A. H. & Martin, B. R. Cannabinoid tolerance and dependence. Handb. Exp. Pharmacol. 168, 691–717 (2005).
Pradhan, A. A. et al. Characterization of a novel model of chronic migraine. Pain 155, 269–274 (2014).
Yamamoto, T. et al. Selective targeting of peripheral cannabinoid receptors prevents behavioral symptoms and sensitization of trigeminal neurons in mouse models of migraine and medication overuse headache. Pain 162, 2246–2262 (2021).
Besnard, J. et al. Automated design of ligands to polypharmacological profiles. Nature 492, 215–220 (2012).
Ramaekers, J. G., Mason, N. L. & Theunissen, E. L. Blunted highs: pharmacodynamic and behavioral models of cannabis tolerance. Eur. Neuropsychopharmacol. 36, 191–205 (2020).
Bass, C. E. & Martin, B. R. Time course for the induction and maintenance of tolerance to Delta(9)-tetrahydrocannabinol in mice. Drug Alcohol Depend. 60, 113–119 (2000).
Henderson-Redmond, A. N. et al. Sex differences in tolerance to delta-9-tetrahydrocannabinol in mice with cisplatin-evoked chronic neuropathic pain. Front. Mol. Biosci. 8, 684115 (2021).
Slivicki, R. A. et al. Impact of Δ9-tetrahydrocannabinol and oxycodone co-administration on measures of antinociception, dependence, circadian activity, and reward in mice. Preprint at bioRxiv https://doi.org/10.1101/2023.12.04.569809 (2023).
Colizzi, M. & Bhattacharyya, S. Cannabis use and the development of tolerance: a systematic review of human evidence. Neurosci. Biobehav. Rev. 93, 1–25 (2018).
D’Souza, D. C. et al. Blunted psychotomimetic and amnestic effects of delta-9-tetrahydrocannabinol in frequent users of cannabis. Neuropsychopharmacology 33, 2505–2516 (2008).
Jones, R. T., Benowitz, N. L. & Herning, R. I. Clinical relevance of cannabis tolerance and dependence. J. Clin. Pharmacol. 21, 143S–152S (1981).
Cuttler, C., Mischley, L. K. & Sexton, M. Sex differences in cannabis use and effects: a cross-sectional survey of cannabis users. Cannabis Cannabinoid Res. 1, 166–175 (2016).
Metna-Laurent, M., Mondésir, M., Grel, A., Vallée, M. & Piazza, P. V. Cannabinoid-induced tetrad in mice. Curr. Protoc. Neurosci. 2017, 9.59.1–9.59.10 (2017).
Zhang, H. et al. Peripherally restricted cannabinoid 1 receptor agonist as a novel analgesic in cancer-induced bone pain. Pain 159, 1814–1823 (2018).
Do, T. P., Hougaard, A., Dussor, G., Brennan, K. C. & Amin, F. M. Migraine attacks are of peripheral origin: the debate goes on. J. Headache Pain 24, 3 (2023).