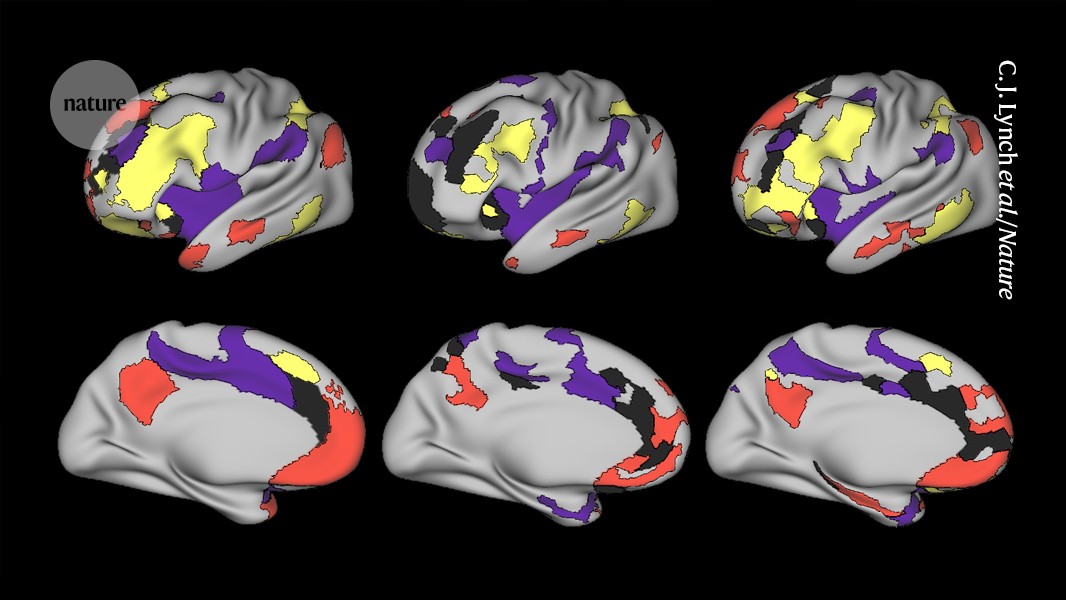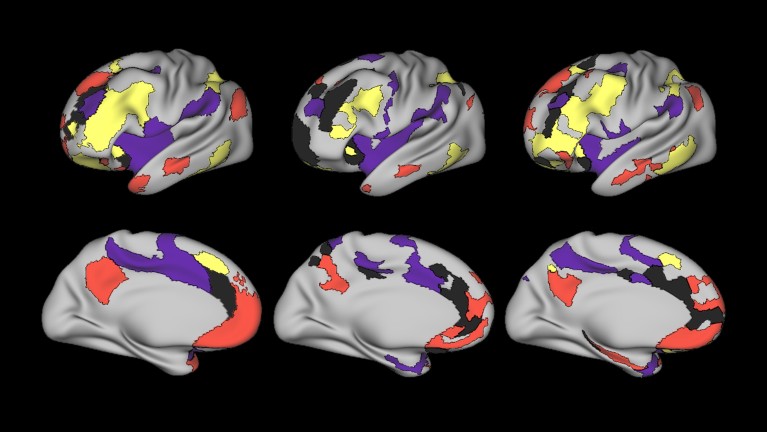
The network of brain cells called the salience network (black) is bigger in people with depression (middle and right columns) than in those without (left column).Credit: C. J. Lynch et al./Nature
The symptoms of depression might come and go, but new evidence suggests that the pattern of brain wiring behind it remains the same for life. The largest imaging study1 of its kind has found that a certain brain network involved in directing attention to stimuli is nearly twice as big in people with depression as it is in the rest of the population — and that it remains that way when a person no longer feels depressed.
The results are a step towards a biological marker for depression, which is at present diagnosed mainly using questionnaires. But the authors say their finding should be validated in more populations before it is used clinically.. The study was published today in Nature.
Networking skills
The technique called functional magnetic resonance imaging (fMRI) allows researchers to study the networks of neurons that wire together different parts of the brain and to measure how much communication passes through these networks. Everyone’s brain networks look fairly similar, but each individual person shows some variation from the average.
Those individual differences are what neuroscientist Charles Lynch and psychiatrist Conor Liston, both at Weill Cornell Medicine in New York City, and their colleagues set out to investigate, hoping to find networks that correlate with depression. But every fMRI scan is just a snapshot of a brain, which limits the technique’s usefulness for studying a dynamic disorder such as depression, Liston says.
The psychedelic escape from depression
So the team turned to existing data sets containing fMRI images of people who had been repeatedly scanned over time: 135 people with major depressive disorder, which causes severe and long-lasting symptoms; and 37 healthy participants. In almost every person with depression, they found, a brain circuit known as the salience network was almost twice as large as it was in controls. The salience network is itself a connector between other brain circuits. It is involved in switching the brain between internal awareness and working memory, and it helps the brain to decide which environmental stimuli and internal emotions it should pay attention to.
At first, the group thought the salience network might expand when a person was depressed. So they used fMRI to scan the brains of several other people with depression nearly every week for up to 18 months and assessed how the person was feeling each time. The salience network of each individual was about the same size every time, whether the person was feeling depressed or not. What did change was the amount of activity between brain regions, which decreased when the person was actively depressed. The researchers could even use network activity to predict whether a person would have a depressive episode the following week.
Early warning sign
The results led the scientists to suspect that a larger network puts people at increased risk of depression, rather than being a simple biomarker for it.
To test this, the team turned to the ABCD Study, which aims to track brain development in nearly 12,000 children between the ages of 9 and young adulthood. They identified 57 children who did not have depression before the age of 13 but who developed the disorder as adolescents. At ages at young as nine years, these children already had expanded salience networks compared with their peers. “It’s moving one step closer to cause and effect,” Liston says.
The researchers are unsure what causes the expansion of the network, but they have a few ideas. Large salience networks could be a genetic trait, given that depression is partly heritable. Alternatively, Lynch says, the network might be overused during a depressive episode — if a person was ruminating on negative stimuli, for instance — and grow in response.
Potential benefits
Diego Pizzagalli, a depression researcher at McLean Hospital in Belmont, Massachusetts, is impressed with the consistency of the findings across databases. If the work is replicated, Pizzagalli says, the size of a child’s salience network could one day be used to identify whether they are at risk of depression, and to intervene through therapy to reduce the likelihood of the disease.
Cognitive neuroscientist Caterina Gratton at the University of Illinois Urbana–Champaign is also impressed with the study, and particularly that it tracked individuals over time instead of looking at large numbers of people. “Rather than reading a few pages of many books, we’re reading whole chapters,” she says.
Lynch says that the team is now investigating whether the expanded network correlates with other mental illnesses that share some symptoms with depression, such as bipolar disorder and obsessive compulsive disorder. “It would be very surprising if this [network expansion] were specific to depression, given how heterogeneous depression is”, he says.