Andrew Moseson experienced severe depression for many years. “Some days I wasn’t able to get out bed. I had long periods of unemployment and was living in my car for a time.” He struggled to find relief, nothing worked. “I tried medications, exercise, volunteering, psychedelics. I read books about happiness, about depression,” he says. “Everything helped a little, but it was still there.” Then, in the spring of 2023, he found a clinical trial that would change his life.
The trial was for people with clinical depression who, like Moseson, had not found success with existing medication. It involved faecal microbiota transplantation (FMT), in which stool from a healthy donor is transferred into a recipient’s gastrointestinal tract to restore a healthy balance of gut bacteria.
The procedure did not work as well for everyone who took part in the trial, but for Moseson the results were transformative — and they came fast. “Within about a week, I started feeling better,” he says. “I felt like my brain was refreshed.”
Nature Outlook: The human microbiome
Two years later, Moseson is still taking his previously prescribed medication. “My doctor doesn’t want me to quit my antidepressants,” he says. “There’s a thought that this transplant could make antidepressants work better.” Whatever the mechanism, the change seems stark. “I feel like I’ve been cured,” Moseson says.
Numerous psychiatric and neurological conditions have been linked to disturbances in people’s gut microbiota — the community of trillions of microorganisms that live symbiotically in the gastrointestinal tract. These are just correlations, but studies in rodents show compelling evidence of causality, and other animal research points to multiple pathways through which the microbiota communicates with the brain.
Moseson’s experience, and others like it, offer preliminary evidence that microbiota-based treatments can be beneficial for people with mood disorders, such as depression and anxiety. The procedure need not be a faecal transplant — good outcomes have also been observed with probiotics (microbial species or strains that have a beneficial effect on the microbiota) and diet. But how these interventions work is not clear. Only with large-scale human trials, including investigation of mechanisms, will researchers be able to say which microbes work, for which conditions, and in which individuals and circumstances.
Transplanting the blues
The trial that Moseson participated in was led by Valerie Taylor, a psychiatrist at the University of Calgary in Canada. Taylor became interested in the gut microbiota after two people with bipolar disorder approached her. “They’d been very sick for a long time and nothing had worked; both took antibiotics, and their symptoms completely changed,” Taylor says. They asked her if there was a link. “I had no idea, but I was going to try to find out.”
Around that time, in 2016, two studies had just been published that showed transferring faecal matter from someone with depression into rodents gave the animals depression-like behaviours1,2. “That was really interesting,” says Taylor. “This is not how we’d thought about mental illness, as something that can be transferred the way you could catch measles.”
One study came from John Cryan, a neurobiologist at University College Cork in Ireland, and his colleagues, who had been looking at the influence of the gut microbiota in stress-related conditions, such as depression and anxiety. They had studied a small sample of people with depression and found that they harboured microbial communities that differed from those of healthy people. But that was just an association. “To prove causality, we wanted to know, if we took that microbiome and put it into a healthy rat, would it do anything?” says Cryan. “Lo and behold, it did.”
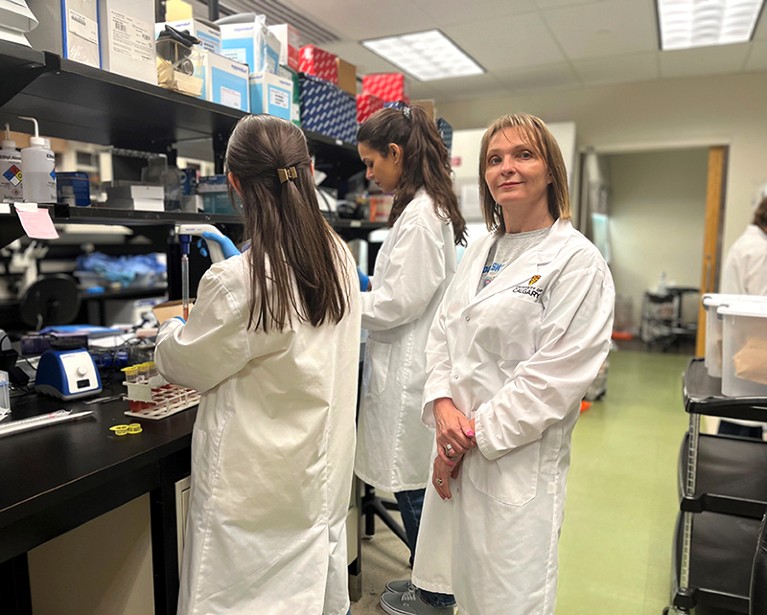
Valerie Taylor, a psychiatrist at the University of Calgary in Canada, is researching how psychiatric illnesses affect the gut microbiota.Credit: Univ. Calgary
Rats that received faecal transplants from people with depression exhibited anhedonia (a lack of interest and pleasure) and anxiety-like behaviours, and had altered metabolism of tryptophan, a precursor to biomolecules such as the neurotransmitter serotonin1. Humans source tryptophan from their diet, because the body doesn’t produce it, and gut microbes help to metabolize it.
The second study, from a team led by researchers at Chongqing Medical University in China, showed the same result in mice, and also noted metabolic changes2.
In December 2023, Cryan and his colleagues showed that symptoms experienced by people with social anxiety disorder could similarly be transferred to rodents through faecal transplants3. Mice that received the transplants showed normal behaviour across a battery of depression and anxiety tests, but showed heightened sensitivity to social fear. This was accompanied by changes in immune function and in the oxytocin system, which plays a crucial part in social behaviour. “This same paradigm of faecal microbiota transplant in animals has been replicated for autism features, and psychosis,” says Viktoriya Nikolova, a psychiatrist at King’s College London.
Evidence of efficacy
These studies inspired Taylor and her colleagues to attempt to translate the findings to human therapies. “We got very interested in whether, if you could transfer illness this way, could you do the reverse?” Taylor says.
Their first trial, which Taylor says is due to be published later this year, was focused on bipolar disorder. Taylor reasoned that if they could make progress in a condition that is generally thought of as highly genetically determined and hard to treat, it should work on other disorders, too. And if anything was going to work in humans, she thought, it would be the comprehensive alterations of the microbiota brought about by FMT, as opposed to tinkering with it by adding a handful of microbial strains. “We needed faecal transplants to see what happens when you completely reset things,” Taylor says. “We thought if we didn’t see anything, we’re not going to do the probiotic work, because it’s probably not going to work either.”
The findings so far have convinced the team to push forwards. They have three more trials at various stages of completion: two focusing on depression, including the one Moseson participated in, and one on obsessive-compulsive disorder. They are also planning another, on attention-deficit hyperactivity disorder.
One drawback of FMT is that it does little to narrow down which microbes are responsible for the benefits. Ultimately, more-targeted treatments could be developed, such as probiotics, but transplant trials could show whether this is worth pursuing.
A handful of small trials of probiotics for depression have found positive effects. In 2021, Nikolova and her colleagues published a meta-analysis of seven such trials4. Five used probiotics in addition to standard-of-care treatments, whereas two trials used them as stand-alone therapies. The analysis found that probiotics — known as psychobiotics when used in this way — are effective as an add-on, but not when used alone. “For now, the best evidence supports psychobiotics as adjunctive therapies,” says Wolfgang Marx, a nutritional psychiatrist at Deakin University in Geelong, Australia. “Something that can complement, rather than replace, standard care.”
In 2023, Nikolova and her colleagues published a pilot trial of 49 people with depression who had previously had only a partial response to antidepressants5. Half of the participants received a multistrain probiotic, in addition to their medication, for eight weeks. This group showed greater reductions in depression and anxiety-related symptoms compared with the placebo group. “What we found was better than expected in terms of clinical efficacy,” says Nikolova.
Researchers have also been investigating whether alterations of the microbiota through diet can be leveraged to improve mental health. A study published in 2017, by a team in Australia, found that an intervention based on a Mediterranean diet reduced symptoms in people with depression6. “Dietary changes affect the broader microbial ecosystem,” says Marx, partly because it introduces many compounds that microbes feed on, known as prebiotics. Although “psychobiotics may be a more targeted approach, diet might offer a more broad-spectrum route to supporting mental health”, he says.
Untangling the web
Despite this preliminary evidence that microbiota-based interventions can influence mood disorders, how they do this remains unclear. Animal studies suggest that there are two-way communication routes between the gut and the brain, and they fall into four broad categories. First, the gut microbiota influences the immune system. Second, microbes in the gut interact with a network formed by the hormone-secreting pituitary and adrenal glands and the hypothalamus, called the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis controls stress responses, mainly by secreting the stress hormone cortisol. Third, microbes also communicate by way of the vagus nerve, which connects the enteric nervous system (a web of neurons that lines the gut) to the brain.
And finally, metabolites produced by microbes can communicate with the brain in various ways. Some do so through the enteric nervous system; others, such as short-chain fatty acids, can slip into the bloodstream and cross the blood–brain barrier to enter the brain directly. Some metabolites influence the synthesis of other molecules that act in the brain, such as neurotransmitters and growth factors. “There’s very good evidence to support all these mechanisms,” says Nikolova.
This web of pathways is collectively called the gut–brain axis, but little is currently known about its relative importance in human illness. “The question is, which pathways are being activated in which disorders, in what relative contribution, at what point in life?” says Cryan.

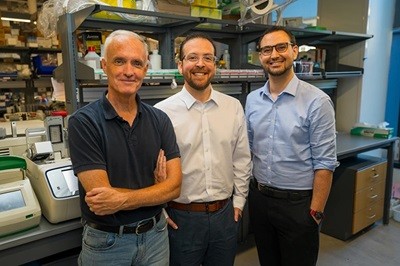
Neurobiologist John Cryan has been studying the effects of the gut microbiota on mental health and stress-related conditions.Credit: Cathal Noonan for Glucksman Gallery, Univ. College Cork
In February, Nikolova and her colleagues published a follow-on study in which they investigated potential mechanisms, but it was inconclusive7. The team collected stool and blood samples to analyse microbiota composition and inflammatory markers. They found no effects on circulating immune-signalling molecules, called cytokines, or on brain-derived neurotrophic factor (BDNF), a growth factor involved in neuronal survival, which some studies4 have implicated in the link between the microbiota and the brain. Several previous trials also failed to find changes in levels of cytokines. All but one study found no significant impact on BDNF4.
The problem might be that, because so many factors affect the microbiota, any effects of probiotics on biomarkers such as immune molecules are drowned out in small samples. “What we need to do next is conduct large-scale clinical trials where we’re studying mechanisms,” Nikolova says. “So we can get a signal above the noise.”
Simply testing all possible candidates isn’t feasible. Researchers don’t yet fully understand what constitutes a healthy microbiota, nor do they have a complete catalogue of human gut microbes. A more tractable approach is to try to understand how probiotics work.
In the follow-on study7 conducted by Nikolova and her colleagues, the most prominent change in participants’ microbiota was an increase in Bacillus bacteria, which correlated with reductions in anxiety symptoms. Generally, changes were transient. Microbial diversity, for instance, was significantly greater in people who received probiotics than in the placebo group after four weeks, but not after eight. Symptoms continued to improve, however, suggesting that benefits might not depend solely on changes in microbiota composition. “It’s telling us this isn’t the only way that [probiotics] have an effect,” says Nikolova.
Researchers now understand that looking only at changes in microbiota composition will not be enough to get to the bottom of how psychobiotics affect mood. “What’s there is interesting, but it’s what they’re doing that’s really important,” says Cryan. One source of uncertainty is that the microbiota has functional redundancy, meaning various microbes can fulfil the same role. “If one species goes down, another might pick up its functions,” says Nikolova. “So it’s not just about what’s missing, but rather whether the function is impaired.”
Understanding all of this will require trials that track as many biomarkers as possible, including immune markers, hormones, neurotransmitters and numerous metabolites, such as short-chain fatty acids and growth factors. Multiomics techniques, which analyse gene activity, proteins, metabolites and more, allow this depth of analysis. These tools were once prohibitively expensive, but decreasing costs are bringing them in reach of more researchers. Trials will also need to account for other factors that can affect microbiota and mental health, such as lifestyle, diet and genetics. “We need large-scale longitudinal studies across the lifespan, combined with brain imaging and other biomarker read-outs that are going to give us real understanding,” says Cryan.
The researchers on a quest to protect the gut from antibiotics
A further complication is that researchers don’t yet fully understand how psychiatric drugs and probiotics interact. Probiotics could work by enhancing the action of antidepressants. Alternatively, if probiotics operate through a different mechanism, they might have separate effects to those medications.
Many common antidepressant drugs target serotonin, and some trials have found that probiotics can increase serotonin synthesis7. This could allow probiotics to augment the action of drugs, such as selective serotonin reuptake inhibitors (SSRIs), and make them a useful add-on to conventional therapy. Probiotics could also boost well-being by mitigating side effects caused by the drugs’ impact on the microbiota, says Nikolova.
However, it is also possible that probiotics have an additive effect. A reduction in the neurotransmitters dopamine and noradrenaline has been linked to depression and anxiety, but SSRIs do nothing to change this. This could partly explain why people with an anxious type of depression typically don’t respond as well to antidepressants. The probiotic that Nikolova and her colleagues used in their trial4,7 included a Bacillus species that produces dopamine and noradrenaline, raising the possibility that the beneficial effects they saw came from targeting different mechanisms to those of participants’ existing medications.
The path ahead
A higher-resolution picture of microbiota changes — and their downstream consequences — will be needed if researchers are to use microbiota data diagnostically. In 2021, Nikolova and her colleagues published a meta-analysis8 of microbiota alterations linked to psychiatric diagnoses. They found that, although increases in pro-inflammatory bacteria and reductions in some anti-inflammatory bacteria were associated with depression, anxiety, bipolar disorder and schizophrenia, the differences did not discriminate between conditions.
Such deeper understanding could even be used for prognosis. “Multiomics approaches are beginning to provide insight into the functional patterns that could predict treatment response or disease risk,” says Marx. “In theory, we could one day personalize psychiatric care based on a person’s microbial and metabolic profile,” he says. But that day has yet to arrive — mainly, says Marx, because “most findings aren’t validated in large clinical cohorts”.
Researchers are struggling to fund large-scale human trials. “The main issue is you can market products without any evidence, the margins are so much lower than in pharma and it’s more difficult to protect, so the incentives aren’t there,” says Cryan. “The flip side is we could democratize health care: by not making these expensive products, we could get them to more people, to socio-economic areas that might benefit most.” Researchers will need to look beyond food and supplement companies. “As a scientist, I need more evidence, but that requires funding through either philanthropic or government sources, we can’t rely on industry to do it.”
Researchers, as well as people with mood disorders, agree this is worthwhile. Moseson is evangelical about the treatment that helped him so much. “Everybody needs to know about this,” he says. His experience changed how he views his depression. “For a long time, I felt ashamed I felt this way, but after the transplant, I started thinking about my depression differently; knowing it wasn’t me, it was my bacteria,” he says. “Then thinking of myself, not just as an individual, but more a collection of biology.”