Bjornevik, K. et al. Longitudinal analysis reveals high prevalence of Epstein–Barr virus associated with multiple sclerosis. Science 375, 296–301 (2022).
Filippi, M. et al. Multiple sclerosis. Nat. Rev. Dis. Primers 4, 43 (2018).
Oksenberg, J. R., Baranzini, S. E., Sawcer, S. & Hauser, S. L. The genetics of multiple sclerosis: SNPs to pathways to pathogenesis. Nat. Rev. Genet. 9, 516–526 (2008).
Bray, P. F., Bloomer, L. C., Salmon, V. C., Bagley, M. H. & Larsen, P. D. Epstein–Barr virus infection and antibody synthesis in patients with multiple sclerosis. Arch. Neurol. 40, 406–408 (1983).
Leibowitz, U. et al. Epidemiological study of multiple sclerosis in Israel. II. Multiple sclerosis and level of sanitation. J. Neurol. Neurosurg. Psychiatry 29, 60–68 (1966).
Angelini, D. F. et al. Increased CD8+ T cell response to Epstein–Barr virus lytic antigens in the active phase of multiple sclerosis. PLoS Pathog. 9, e1003220 (2013).
Lünemann, J. D. et al. Increased frequency and broadened specificity of latent EBV nuclear antigen-1-specific T cells in multiple sclerosis. Brain 129, 1493–1506 (2006).
Lanz, T. V. et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature 603, 321–327 (2022).
Bar-Or, A. et al. Rituximab in relapsing-remitting multiple sclerosis: a 72-week, open-label, phase I trial. Ann. Neurol. 63, 395–400 (2008).
Hauser, S. L. et al. B-cell depletion with rituximab in relapsing-remitting multiple sclerosis. N. Engl. J. Med. 358, 676–688 (2008).
Hauser, S. L. et al. Ocrelizumab versus interferon β-1a in relapsing multiple sclerosis. N. Engl. J. Med. 376, 221–234 (2017).
Rubtsova, K. et al. B cells expressing the transcription factor T-bet drive lupus-like autoimmunity. J. Clin. Invest. 127, 1392–1404 (2017).
Punnanitinont, A. et al. TLR7 activation of age-associated B cells mediates disease in a mouse model of primary Sjogren’s disease. J. Leukoc. Biol. 115, 497–510 (2024).
Tsubaki, T. et al. Accumulation of plasma cells expressing CXCR3 in the synovial sublining regions of early rheumatoid arthritis in association with production of Mig/CXCL9 by synovial fibroblasts. Clin. Exp. Immunol. 141, 363–371 (2005).
Fox, R. I., Luppi, M., Kang, H. I. & Pisa, P. Reactivation of Epstein–Barr virus in Sjogren’s syndrome. Springer Semin. Immunopathol. 13, 217–231 (1991).
James, J. A. et al. Systemic lupus erythematosus in adults is associated with previous Epstein–Barr virus exposure. Arthritis Rheum. 44, 1122–1126 (2001).
Alspaugh, M. A., Jensen, F. C., Rabin, H. & Tan, E. M. Lymphocytes transformed by Epstein–Barr virus. Induction of nuclear antigen reactive with antibody in rheumatoid arthritis. J. Exp. Med. 147, 1018–1027 (1978).
SoRelle, E. D. et al. Time-resolved transcriptomes reveal diverse B cell fate trajectories in the early response to Epstein–Barr virus infection. Cell Rep. 40, 111286 (2022).
Mouat, I. C. et al. Gammaherpesvirus infection drives age-associated B cells toward pathogenicity in EAE and MS. Sci. Adv. 8, eade6844 (2022).
Miller, G. & Lipman, M. Comparison of the yield of infectious virus from clones of human and simian lymphoblastoid lines transformed by Epstein–Barr virus. J. Exp. Med. 138, 1398–1412 (1973).
Miller, G. & Lipman, M. Release of infectious Epstein–Barr virus by transformed marmoset leukocytes. Proc. Natl Acad. Sci. USA 70, 190–194 (1973).
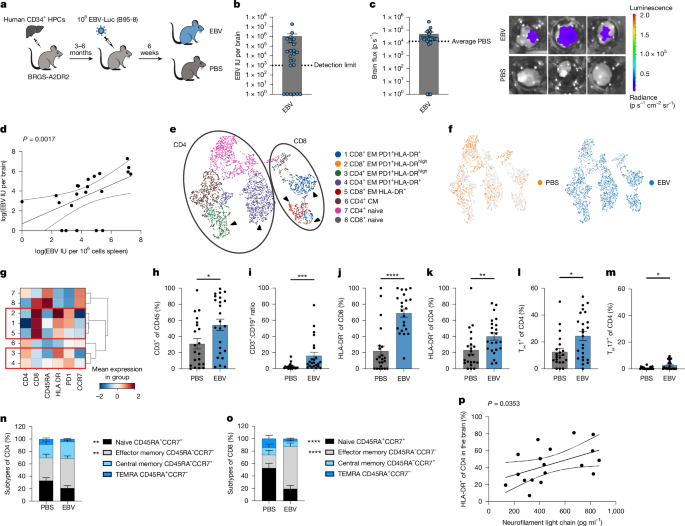
Zdimerova, H. et al. Attenuated immune control of Epstein–Barr virus in humanized mice is associated with the multiple sclerosis risk factor HLA-DR15. Eur. J. Immunol. 51, 64–75 (2021).
van Langelaar, J. et al. Induction of brain-infiltrating T-bet-expressing B cells in multiple sclerosis. Ann. Neurol. 86, 264–278 (2019).
Jain, R. W. & Yong, V. W. B cells in central nervous system disease: diversity, locations and pathophysiology. Nat. Rev. Immunol. 22, 513–524 (2022).
SoRelle, E. D. et al. An EBV-associated atypical B cell signature in clinically isolated syndrome is implicated in progression of multiple sclerosis. Preprint at medRxiv https://doi.org/10.1101/2023.02.26.23286433 (2024).
Fournier, B. et al. Inherited TNFSF9 deficiency causes broad Epstein–Barr virus infection with EBV+ smooth muscle tumors. J. Exp. Med. 219, e20211682 (2022).
Baranzini, S. E. et al. B cell repertoire diversity and clonal expansion in multiple sclerosis brain lesions. J. Immunol. 163, 5133–5144 (1999).
Yang, X. et al. Liquid–liquid phase separation of RBM33 facilitates hippocampus aging by inducing microglial senescence by activating CDKN1A. Int. J. Biol. Macromol. 310, 142986 (2025).
Evans, A. K. et al. Impact of noradrenergic inhibition on neuroinflammation and pathophysiology in mouse models of Alzheimer’s disease. J. Neuroinflammation 21, 322 (2024).
Reali, C. et al. B cell rich meningeal inflammation associates with increased spinal cord pathology in multiple sclerosis. Brain Pathol. 30, 779–793 (2020).
Choi, S. R. et al. Meningeal inflammation plays a role in the pathology of primary progressive multiple sclerosis. Brain 135, 2925–2937 (2012).
McHugh, D. et al. EBV renders B cells susceptible to HIV-1 in humanized mice. Life Sci. Alliance 3, e202000640 (2020).
White, R. E. et al. EBNA3B-deficient EBV promotes B cell lymphomagenesis in humanized mice and is found in human tumors. J. Clin. Invest. 122, 1487–1502 (2012).
Münz, C. Latency and lytic replication in the oncogenesis of the Epstein Barr virus. Nat. Rev. Microbiol. 17, 691–700 (2019).
Babcock, J. G., Hochberg, D. & Thorley-Lawson, A. D. The expression pattern of Epstein–Barr virus latent genes in vivo is dependent upon the differentiation stage of the infected B cell. Immunity 13, 497–506 (2000).
SoRelle, E. D., Reinoso-Vizcaino, N. M., Horn, G. Q. & Luftig, M. A. Epstein–Barr virus perpetuates B cell germinal center dynamics and generation of autoimmune-associated phenotypes in vitro. Front. Immunol. 13, 1001145 (2022).
Hochberg, D. et al. Demonstration of the Burkitt’s lymphoma Epstein–Barr virus phenotype in dividing latently infected memory cells in vivo. Proc. Natl Acad. Sci. USA 101, 239–244 (2004).
Nowag, H. et al. Macroautopphagy proteins assist Epstein Barr virus production and get incorporated into the virus particles. EBioMedicine 1, 116–125 (2014).
Lünemann, J. D. et al. EBNA1-specific T cells from patients with multiple sclerosis cross react with myelin antigens and co-produce IFN-γ and IL-2. J. Exp. Med. 205, 1763–1773 (2008).
Serafini, B., Rosicarelli, B., Veroni, C., Mazzola, G. A. & Aloisi, F. Epstein–Barr virus-specific CD8 T cells selectively infiltrate the brain in multiple sclerosis and interact locally with virus-infected cells: clue for a virus-driven immunopathological mechanism. J. Virol. https://doi.org/10.1128/JVI.00980-19 (2019).
Gottlieb, A., Pham, H. P. T., Saltarrelli, J. G. & Lindsey, J. W. Expanded T lymphocytes in the cerebrospinal fluid of multiple sclerosis patients are specific for Epstein–Barr-virus-infected B cells. Proc. Natl Acad. Sci. USA 121, e2315857121 (2024).
Thomas, O. G. et al. Cross-reactive EBNA1 immunity targets α-crystallin B and is associated with multiple sclerosis. Sci. Adv. 9, eadg3032 (2023).
Tengvall, K. et al. Molecular mimicry between anoctamin 2 and Epstein–Barr virus nuclear antigen 1 associates with multiple sclerosis risk. Proc. Natl Acad. Sci. USA 116, 16955–16960 (2019).
Sahir, F., Mateo, J. M., Steinhoff, M. & Siveen, K. S. Development of a 43 color panel for the characterization of conventional and unconventional T-cell subsets, B cells, NK cells, monocytes, dendritic cells, and innate lymphoid cells using spectral flow cytometry. Cytometry A https://doi.org/10.1002/cyto.a.24288 (2020).
Puccio, S. et al. CRUSTY: a versatile web platform for the rapid analysis and visualization of high-dimensional flow cytometry data. Nat. Commun. 14, 5102 (2023).
Adhikary, D. et al. Immunodominance of lytic cycle antigens in Epstein–Barr virus-specific CD4+ T cell preparations for therapy. PLoS ONE 2, e583 (2007).
Nuckel, J. et al. Association between IgG responses against the nucleocapsid proteins of alphacoronaviruses and COVID-19 severity. Front. Immunol. 13, 889836 (2022).
Soldan, S. S. et al. Epigenetic plasticity enables CNS-trafficking of EBV-infected B lymphocytes. PLoS Pathog. 17, e1009618 (2021).
Oner, A. & Kobold, S. Transwell migration assay to interrogate human CAR-T cell chemotaxis. STAR Protoc. 3, 101708 (2022).
Fennell, E. Single-cell RNA and B cell receptor sequencing processed data from EBV-infected and PBS humanised BRGS-A2DR2 mice. Zenodo https://doi.org/10.5281/zenodo.15602185 (2025).
Fennell, E. Multiplex immunofluorescence images of spleens from EBV-infected BRGS-A2DR2 mice. Zenodo https://doi.org/10.5281/zenodo.15599580 (2025).