Close to 110,000 heat-related deaths are estimated to have occurred in Europe during the summers of 2022 and 2023 combined1. That’s roughly the same number of people as if a fully occupied jumbo jet crashed every day for 16 weeks. Meanwhile, a vast array of heat-related impacts disrupt people’s lives. Hot weather worsens mental-health problems2, increases the likelihood of violence3 and makes pregnant women more likely to give birth prematurely4. In classrooms, it impairs children’s ability to learn5.
Shade is an essential solution for hotter cities
The problems are expected to get much worse. Without better adaptation, heat-related deaths are projected to rise 3.7-fold by mid-century if global temperatures reach 2 °C above pre-industrial levels6. (In 2024, the average global temperature exceeded 1.5 °C above pre-industrial levels for the first time.) And heat stress in the workplace is expected to cost the global economy US$2.4 trillion each year in lost productivity by 2030.
Currently, most approaches that alert the public to heat-health risk worldwide use ambient (air) temperature thresholds to trigger warnings — usually broad recommendations to reduce activity, stay hydrated and so on. These thresholds are generally based on overall statistical correlations between ambient temperatures and regional increases in death and disease7. But heat stress is defined by more than just temperature, and can affect multiple physiological systems, including the heart and kidneys4. The risk to individuals varies enormously, and depends on factors such as their age, the health of their kidneys and heart, what they are wearing and their level of activity.
Two of us (O.J. and F.T.) are piloting the integration of physiological models and weather data to estimate people’s ‘heat-health risk’. We think that heat adaptation could be vastly enhanced by using a physiology-based approach that focuses on hot people, rather than just on hot weather.
How hot is too hot?
Most people can safely tolerate core body temperatures of up to about 39 °C. If body temperature exceeds this value, the risk of heat exhaustion increases, with symptoms including nausea, dizziness and vomiting. At core temperatures above 40 °C, heat stroke can occur. Here, an increase in gut permeability, caused by reduced delivery of oxygen by the blood, allows toxic molecules associated with certain bacteria to leak into the bloodstream. This can trigger an inflammatory response that cascades to cause blood clotting, multiple organ failure and, ultimately, death4.

Water sprays from a crane to help cool down construction workers in Nanjing, China, during high temperatures last month.Credit: Liu Jianhua/VCG via Getty
Whether and how much any one person is harmed by hot weather depends on a mix of environmental factors and characteristics specific to that individual. Besides air temperature, three features of the thermal environment are important: radiation, humidity and wind speed8. Someone in direct sunlight can be exposed to mean radiant temperatures that are more than 20 °C greater than shade temperatures. (Air temperatures used to trigger health warnings are measured in the shade.) High humidity and low wind speed impair the effectiveness of sweating, which is a person’s only effective physiological cooling mechanism at air temperatures above 35 °C. The ability to lose heat through the evaporation of sweat is also affected by the thermal and evaporative properties of clothing8, age, body size and some medications9. Even light activity such as walking more than doubles internal heat production, and so increases a person’s risk of experiencing health problems in hot weather.
The body’s thermoregulation is underpinned by a vast redistribution of blood to the skin. And in hot weather, the need to lose heat increases, meaning that to maintain blood pressure, the heart must pump more often and with greater force. People with heart disease are less able to compensate for the increased strain, and so face higher cardiovascular risk4. The redistribution of blood can also damage organs such as the kidneys by reducing how much oxygen is delivered to them. A depleted blood volume from dehydration in hot weather forces the heart to work harder still, and repeated dehydration can contribute to kidney fibrosis (the accumulation of scar tissue in the kidney) and chronic kidney disease4. People with kidney disease face a higher risk of renal failure in extreme heat.
A physiology-based approach
When air temperatures are expected to exceed a certain threshold, warnings are triggered that help to prepare health and energy systems for bouts of extreme heat1. But the health-related warnings are limited by the quality of available data on heat-related deaths and disease10, and they don’t enable precise tailoring of protective measures for groups that are at higher risk.
Why we still don’t know the mounting health risks of climate change
The narrow focus on air temperature also strengthens an entrenched belief that reducing ambient temperatures is the only way to lessen the impacts of heat on health11. But attempts to do this can be unsustainable or ineffective. Coating hot surfaces such as roads with reflective paint, for example, will probably have little impact on physiological heat strain or even on perceived discomfort unless people are lying on the ground, and might even intensify heat loads on people. The benefit of increasing green areas and tree cover in cities is similarly often evaluated according to how much it can reduce the temperature of pavements or the mean air temperature, even though the main thermal benefit of urban greening is increasing people’s access to shade.
In a physiology-based approach, all the parameters with sufficiently high-quality data can be integrated into models to estimate three factors: a person’s core body temperature, their level of dehydration and the strain on their heart and circulatory system8. In our pilot studies in Sydney, Australia, we incorporated six parameters: ambient temperature, thermal radiation level, humidity level, wind speed, a person’s level of activity and the thermal and evaporative properties of their clothing. (Physiological acclimatization — the well-understood physiological adjustments that occur when a person is repeatedly exposed to a hot environment — can also be incorporated.)
Estimates of physiological strain can then be compared with long-established physiological safety thresholds for different groups, on the basis of characteristics such as age, whether the person has a pre-existing condition, what medications they are taking and so on. For example, people with coronary artery disease can tolerate much less cardiovascular strain than healthy individuals can12, and those with heart failure or kidney disease can tolerate less dehydration. The final aggregated score is an individual’s ‘heat-health risk’ (see ‘Assessing heat-induced health risks using physiology’).
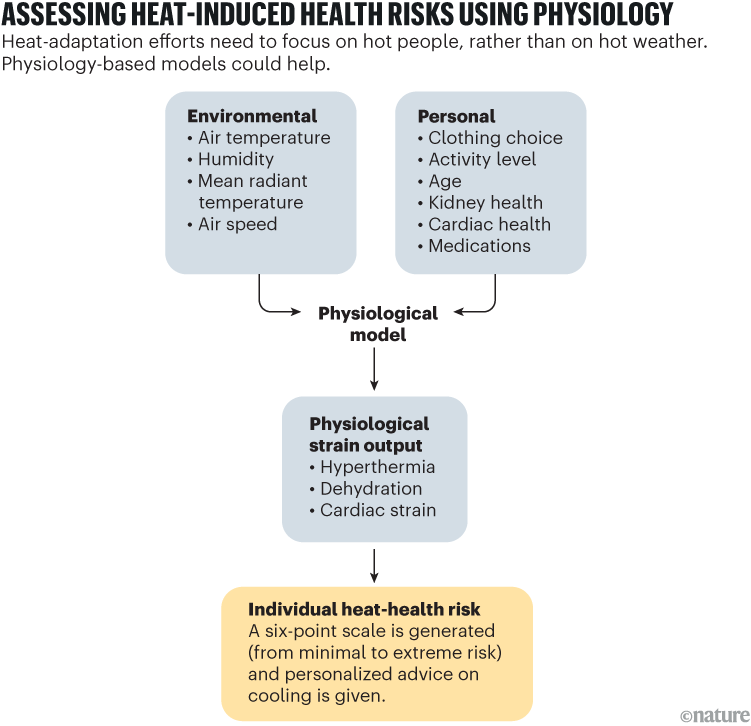
Source: O. Jay et al.
Making it happen
The physiological and biophysical models needed for this sort of approach are already available. To provide individuals with a personalized rating of heat-stress risk that uses a six-point scale, two of us (O.J. and F.T.) have developed a freely available Internet tool called HeatWatch (see go.nature.com/44ymweq). This allows users to create personal profiles by submitting their age, related health conditions, medications, access to air conditioning and so on. It then provides a seven-day forecast of heat-health risk and provides evidence-based cooling advice tailored to each profile.
Ultimately, we plan to develop an online interface similar to the dashboards that tracked people’s risk of infection with the coronavirus SARS-CoV-2 during the COVID-19 pandemic. Such an interface could allow governments, public-health organizations, policymakers and others to better anticipate where and when certain groups will face elevated heat-health risks. This should make measures to reduce those risks, such as the deployment of pop-up cooling hubs for people who are homeless, more targeted and cost-effective.

A hospital in New Delhi has a specialized unit for treating people who have heat stroke.Credit: Vipin Kumar/Hindustan Times via Getty




