Alzheimer’s disease has long eluded treatment. Attempts to tackle it by targeting the amyloid-β protein that accumulates in the brains of people with the condition have often foundered on the rocks of clinical testing. Between 2004 and 2021, 14 different compounds that directly target amyloid-β failed to make it through phase III trials. This led some researchers to question the theory behind the prospective drugs’ development: that amyloid-β is the trigger for a chain of biochemical and cellular events that leads to neurodegeneration and dementia.
In the past few years, however, it seems that these efforts have begun to pay off. Since 2021, three anti-amyloid drugs have received regulatory approval in the United States for treating Alzheimer’s disease. The first, aducanumab, was mired in controversy and has been withdrawn, but trials published in 2022 and 2023 showed clearly that two others, lecanemab and donanemab, slowed cognitive decline1,2.
Nature Outlook: Alzheimer’s disease
The drugs are antibodies that clear away plaques of amyloid-β in the brain, and for many researchers their success puts to bed the argument that the theory guiding almost all Alzheimer’s drug development so far is incorrect. “At one level, I think the amyloid hypothesis is proven,” says John Hardy, a neurogeneticist at University College London who pioneered the theory. “We remove amyloid, and we slow the disease process.”
But dissent persists. The drugs’ effects are modest, sparking debate about whether the benefits are meaningful enough to justify the high cost and risk of side effects. Proponents argue that this is just the beginning — avenues are now open to reduce side effects, increase efficacy and combine the drugs with other therapeutics. But some researchers are still questioning whether clearing away amyloid-β plaques will ever be enough to halt the disease, or whether there might be other, potentially better, targets in the brain. “The question is, what do these results really mean?” says David Rubinsztein, a neurogeneticist at the University of Cambridge, UK. “It might be the thin end of the wedge, or it might be as good as we’re going to get. Frankly, I don’t think we know.”
Risk and reward
Lecanemab was approved by the US Food and Drug Administration (FDA) in 2023 and donanemab in 2024. Both slow cognitive decline by around 30%. Whether this is clinically meaningful has been hotly debated; some clinicians argue that individuals will not notice a difference, but others say that even a moderate slow down delivers real benefit to a person with the disease and their family. “A 30% less-steep decline does mean something,” says Charlotte Teunissen, a neuroscientist at Amsterdam University Medical Center. Even six months longer in a coherent state, she says, “is the difference between being able to have meaningful conversations with your children about their lives, or not”.
The drugs also have side effects, which are occasionally serious. Reducing these will be key to shifting the risk–benefit equation in the drugs’ favour. In the pivotal trial of lecanemab1, 21.5% of people treated developed brain swelling or bleeding, collectively known as amyloid-related imaging abnormalities (ARIA). This is usually asymptomatic, but around one-quarter of people with ARIA experience confusion, headaches or dizziness. Seizures and even death are rarer, but not unheard of.
Brain bleeds are thought to be caused by antibodies binding to amyloid-β in blood vessels, and swelling is thought to be due to neuroinflammatory reactions. Unfortunately, an inflammatory reaction — when the brain’s main immune cells, called microglia, switch into a pro-inflammatory state — is how many researchers think that these drugs work. Activated microglia hoover up plaques, so the benefits and side effects could be difficult to separate. Currently, the higher the dose, the greater the ARIA risk, presenting a potential trade-off between efficacy and safety.
A delivery approach called a brain shuttle could shift this balance. This technique exploits receptors for the protein transferrin on epithelial cells of the blood–brain barrier that typically ferry iron into the brain. If a transferrin molecule is attached to an anti-amyloid antibody, these receptors can then shuttle the combined molecule across the barrier, moving the drug into the brain from the circulation more efficiently than would otherwise be possible. “A higher concentration gets into the brain, so you can lower the dose to get the same effect,” says Teunissen. A drug that uses this mechanism, trontinemab, is in early-stage trials. “The first results are very promising; they have lower ARIA rates and quick amyloid reduction,” she says.
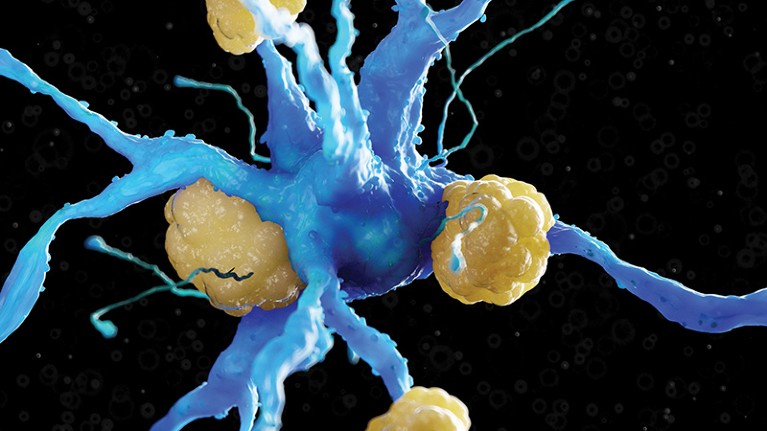
Illustration of amyloid-β on a nerve cell.Credit: Sebastian Kaulitzki/ Science Photo Library/ Getty Images
As well as improving safety, another important factor in maximizing the potential of anti-amyloid antibodies will be expanding access to under-served groups. “The people who get treated with these antibodies at clinics are largely well-educated, well-heeled people who aren’t representative of the breadth of society,” says Dennis Selkoe, a neurologist at Brigham and Women’s Hospital in Boston, Massachusetts. Simpler methods of administering the drugs would help. Currently, people have to travel to clinics for intravenous infusions once or twice a month, but multiple companies are formulating versions that can instead be injected under the skin — something a nurse or family member could assist with at home, Selkoe says. “That’ll probably happen in 2025 or 2026.”
Researchers are also exploring the possibility of using these drugs earlier in the course of the disease. Amyloid-β begins accumulating in the brain 20–30 years before symptoms appear. By this point, events that occur later in the chain of pathology might have been triggered already and could continue regardless of amyloid-β clearance. Data from failed trials and the recent successes suggest that anti-amyloid antibodies are of little clinical benefit once a person has progressed beyond mild dementia, regardless of how well plaques are cleared.
Two ongoing trials — Ahead and Trailblazer-Alz 3 — are testing whether the drugs can prevent the onset of symptoms in people who aren’t experiencing cognitive effects but in whom amyloid-β has started to accumulate. “Prevention for Alzheimer’s, at least in some people, is close now,” says Selkoe. “It’ll be an historic event if we can show that people who have Alzheimer’s pathology do not progress to significant forgetfulness.”
If the drugs prove to be more effective when administered before symptoms develop, advances in monitoring the development of pathology using biomarkers in the blood might be key to identifying, cheaply, people who would benefit from preventive treatment.
The next generation
As well as making better use of existing anti-amyloid drugs, researchers are developing what could be the next phase of this therapeutic approach.
Rather than deliver ready-made antibodies, one line of work is to prompt the body to produce its own, using an amyloid-β vaccine. This would be straightforward to administer and cheaper than antibody infusions. “To get to large numbers of people who don’t normally make it into academic medical centres, you need something simple and safe,” Selkoe says.
An early attempt to make this work was abandoned in 2002 after some trial participants developed inflammation of the brain and the membranes that surround it. But now, armed with an understanding of why this happened (part of the vaccine provoked a response by a type of white blood cell called a T cell) and how to avoid it, researchers are returning to the concept. “It’s not ready for primetime, but there are active attempts to design vaccination studies,” says Selkoe.
If a vaccine were developed, it would probably be used to prevent familial Alzheimer’s in people who carry mutations that cause early-onset disease. People with mutations such as APOE4, which increase the risk of the more common sporadic form of the disease, might also be candidates.
Another focus is to target the disease process even earlier, and prevent the build-up of amyloid-β plaques in the first place. Amyloid-β is a fragment of a larger protein called amyloid precursor protein (APP) that crosses cell membranes. Two enzymes — first β-secretase, then γ-secretase — slice APP in two places, creating amyloid-β. Small molecules to target these enzymes could stop plaques from forming.
Researchers have tried inhibiting γ-secretase, but blocking the enzyme completely proved to be a bad idea because it has other biological functions. “There were a lot of side effects,” says Bart De Strooper, a neuroscientist at the UK Dementia Research Institute in London. “The whole field panicked and decided not to move that forward.” Now, rather than blocking γ-secretase completely, the focus is instead on influencing how and at what point the enzyme cuts APP. “γ-secretase modulators are the future of amyloid therapy,” De Strooper says.
Mutations in three genes that can cause familial Alzheimer’s disease are known to affect APP processing, and result in the production of more or longer strings of amyloid-β. These longer proteins are more prone to clumping in plaques than are shorter forms, leading some researchers to think that tipping the balance in favour of short lengths of amyloid-β could be of benefit. “The long forms catalyse aggregation, so we need to shift the ratio of long over short,” says De Strooper.
Experimental γ-secretase modulators have had issues with liver and kidney toxicity, but a drug in development at Swiss pharmaceutical company Roche is showing promise in early-stage trials. “They didn’t see any mechanistic side effects, and the toxicity seems to be overcome,” says De Strooper. If this approach proves effective, it could make a cheap, daily oral pill possible. “In the fullness of time, γ-secretase modulators will become the statin of Alzheimer’s disease,” says Selkoe.
Multiple targets
Although they get the lion’s share of attention, amyloid-β plaques are not the only targets for Alzheimer’s therapies that are under development. Indeed, many researchers think that the most effective treatment strategy will be to target multiple aspects of the disease at once.
As well as amyloid-β plaques, Alzheimer’s is also characterized by tangles of the protein tau that accumulate inside neurons. Most people think that amyloid-β pathology triggers the development of tau tangles, but that does not necessarily mean that clearing away amyloid-β will put the brakes on tau as well. At a certain point, tau pathology might become self-sustaining and continue to develop regardless. “You can remove amyloid, but you won’t stop that process,” says De Strooper.
Biomarker analyses have also shown that the location and amount of tau pathology correlates more closely with the type and severity of a person’s symptoms than do those of amyloid-β plaques. Tau is therefore usually seen as the most important next treatment target. Various potential anti-tau therapies are in early-stage trials, including antibodies, a vaccine, small molecules and DNA-based techniques.
Trials of therapeutic regimes that combine these approaches with amyloid-targeting therapies are already under way. The Alzheimer’s tau platform (ATP) trial, for example, will test multiple tau-targeted therapies both alone and combined with an anti-amyloid drug. Similarly, Roche is combining its in-development γ-secretase modulator with lecanemab.
All these ideas broadly align with the amyloid hypothesis of Alzheimer’s, which states that amyloid-β accumulation is the first step in the disease and the initial trigger for cell death. But another theory that is beginning to gain acceptance suggests that there could be an even earlier target for intervention: dysfunction of lysosomes, the cells’ waste-clearance machinery. “It’s an important alternative hypothesis that needs to be part of the puzzle we’re trying to solve,” says Rubinsztein.

Ralph Nixon has pioneered an alternative theory for Alzheimer’s.Credit:Karen Dias/ Quanta Magazine
Multiple labs have found that in Alzheimer’s disease, lysosomes become enlarged and dysfunctional even before plaques appear. So do endosomes, another part of cells’ waste-clearance apparatus. The idea is that this disposal failure causes waste — including amyloid-β — to accumulate inside cells, ultimately killing them and spilling ready-made plaques into the brain. “Maybe what’s going on in the trials is you’re removing an irritant, which has a small effect,” says Rubinsztein. “But the primary cause of cell death is lysosomal dysfunction, not amyloid-β.”
A group led by Ralph Nixon, a neurobiologist at New York University who pioneered this theory, has found evidence of bulging neurons with swollen lysosomes spilling waste into the brain in both mice and brain tissue from people with Alzheimer’s disease. The crux of this dysfunction seems to be impaired regulation of lysosomes’ pH, leaving them insufficiently acidic to degrade molecules.
Nixon and his colleagues have shown in mouse models3 that drugs that re-acidify lysosomes result in fewer amyloid-β plaques and less cell death. Such drugs already exist for use in other disorders. Now, Nixon’s group is developing versions that can cross into the brain more easily and have fewer side effects, meaning that they might be suitable for use in people with Alzheimer’s.
Course correction
Nixon’s findings challenge the idea that amyloid-β plaques should be the main target for Alzheimer’s therapies. A key realization that underpins this is that the same mutations that affect amyloid-β production also affect lysosomes. “Most genes do many things,” says Rubinsztein.
Nixon and his colleagues have suggested that the fragment of APP that remains in the cell membrane after β-secretase cleaves APP, known as APP-βCTF, interferes with pumps that regulate lysosomal pH4,5. Mutations in the APP gene that is responsible for some forms of familial Alzheimer’s cause too much APP-βCTF to be produced. Another mutation, in the PSEN1 gene that causes certain types of familial Alzheimer’s, also interferes with these pumps.
More from Nature Outlooks
The standard model of Alzheimer’s assumes that amyloid-β plaques form and kill neurons from outside, but the work by Nixon and his colleagues is part of a growing body of evidence suggesting the opposite. “More people are starting to agree that the disease starts inside the cell, rather than outside,” says Nixon.
Even stalwarts of the amyloid hypothesis think that Nixon is on to something. “He’s been saying there’s something wrong in the endosome-lysosome pathway for a long time,” says Hardy. “With very convincing evidence.” Although Hardy still thinks that familial disease is caused by the overproduction of amyloid-β, he agrees that sporadic Alzheimer’s is mainly a problem of clearance. But while Nixon’s work implicates lysosomes, Hardy blames microglia, mainly because gene-association studies strongly implicate microglia in sporadic Alzheimer’s disease. Nixon, however, contends that these cells come into play later in the course of the disease. “Microglia clear extracellular amyloid, but we’d say this mainly occurs after it’s released from dying cells,” he says.
The consequences for future treatments are significant. If Nixon is right, then, just as vacuuming up wood dust from the floor won’t solve the problem of termites in your wall, clearing amyloid-β plaques will never halt the disease, because it doesn’t address the underlying problem. It might make you feel better in the short term, he says, just as removing dust might help a person to breathe more easily — but no more than that. Others see the logic in this thinking. “If the clearance mechanisms are the primary things that go wrong, then we’ve got to rescue them,” says Rubinsztein.
Today’s plaque-clearing anti-amyloid drugs are a valuable and significant step forward. But as understanding of the disease grows, so does the feeling that stopping Alzheimer’s might require treatments that do more than these antibodies can.