Talbott, H. E., Mascharak, S., Griffin, M., Wan, D. C. & Longaker, M. T. Wound healing, fibroblast heterogeneity, and fibrosis. Cell Stem Cell 29, 1161–1180 (2022).
Wynn, T. A. Fibrotic disease and the TH1/TH2 paradigm. Nat. Rev. Immunol. 4, 583–594 (2004).
Glasser, S. W. et al. Mechanisms of lung fibrosis resolution. Am. J. Pathol. 186, 1066–1077 (2016).
Glassberg, M. K. Overview of idiopathic pulmonary fibrosis, evidence-based guidelines, and recent developments in the treatment landscape. Am. J. Manag. Care 25, S195–S203 (2019).
Michalski, J. E., Kurche, J. S. & Schwartz, D. A. From ARDS to pulmonary fibrosis: the next phase of the COVID-19 pandemic? Transl. Res. 241, 13–24 (2022).
Xie, T. et al. Single-cell deconvolution of fibroblast heterogeneity in mouse pulmonary fibrosis. Cell Rep. 22, 3625–3640 (2018).
Tsukui, T. et al. Collagen-producing lung cell atlas identifies multiple subsets with distinct localization and relevance to fibrosis. Nat. Commun. 11, 1920 (2020).
Adams, T. S. et al. Single-cell RNA-seq reveals ectopic and aberrant lung-resident cell populations in idiopathic pulmonary fibrosis. Sci. Adv. 6, eaba1983 (2020).
Kheirollahi, V. et al. Metformin induces lipogenic differentiation in myofibroblasts to reverse lung fibrosis. Nat. Commun. 10, 2987 (2019).
Mascharak, S. et al. Desmoplastic stromal signatures predict patient outcomes in pancreatic ductal adenocarcinoma. Cell Rep. Med. 4, 101248 (2023).
Foster, D. S. et al. Multiomic analysis reveals conservation of cancer-associated fibroblast phenotypes across species and tissue of origin. Cancer Cell 40, 1392–1406.e7 (2022).
Mascharak, S. et al. Preventing Engrailed-1 activation in fibroblasts yields wound regeneration without scarring. Science 372, eaba2374 (2021).
Coelho, P. G. B., de Souza, M. V., Conceição, L. G., Viloria, M. I. V. & Bedoya, S. A. O. Evaluation of dermal collagen stained with picrosirius red and examined under polarized light microscopy. An. Bra. Dermatol. 93, 415–418 (2018).
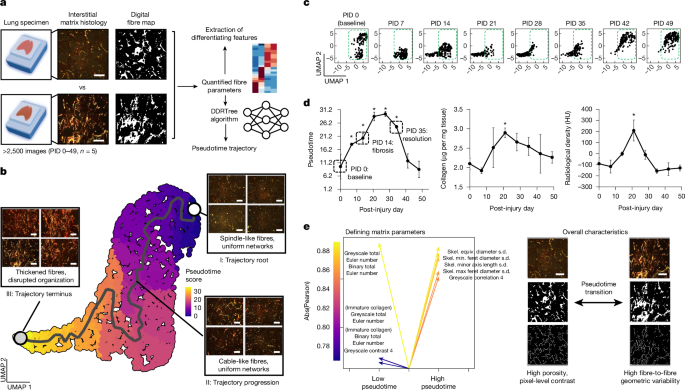
Mao, Q., Wang, L., Goodison, S. & Sun, Y. Dimensionality reduction via graph structure learning. In Proc. 21st ACM SIGKDD Conference on Knowledge Discovery and Data Mining (eds Cao, L. & Zhang, C.) 765–774 (2015).
Trapnell, C. et al. Pseudo-temporal ordering of individual cells reveals dynamics and regulators of cell fate decisions. Nat. Biotechnol. 32, 381 (2014).
Organ, L. A. et al. Biomarkers of collagen synthesis predict progression in the PROFILE idiopathic pulmonary fibrosis cohort. Resp. Res. 20, 148 (2019).
Jin, S. et al. Inference and analysis of cell–cell communication using CellChat. Nat. Commun. 12, 1088 (2021).
Morse, C. et al. Proliferating SPP1/MERTK-expressing macrophages in idiopathic pulmonary fibrosis. Eur. Resp. J. 54, 1802441 (2019).
Shen, M., Luo, Z. & Zhou, Y. Regeneration-associated transitional state cells in pulmonary fibrosis. Int. J. Mol. Sci. 23, 6757 (2022).
Enomoto, Y. et al. LTBP2 is secreted from lung myofibroblasts and is a potential biomarker for idiopathic pulmonary fibrosis. Clin. Sci. 132, 1565–1580 (2018).
Travaglini, K. J. et al. A molecular cell atlas of the human lung from single-cell RNA sequencing. Nature 587, 619–625 (2020).
Wang, S. et al. S100A8/A9 in inflammation. Front. Immunol. 9, 1298 (2018).
Cui, L. et al. Activation of JUN in fibroblasts promotes pro-fibrotic programme and modulates protective immunity. Nat. Commun. 11, 2795 (2020).
Guan, R. et al. Bone morphogenetic protein 4 inhibits pulmonary fibrosis by modulating cellular senescence and mitophagy in lung fibroblasts. Eur. Resp. J. 60, 2102307 (2022).
Buschman, M. D. & Field, S. J. MYO18A: an unusual myosin. Adv. Biol. Reg. 67, 84–92 (2018).
Wang, L. et al. CCAAT/enhancer-binding proteins in fibrosis: complex roles beyond conventional understanding. Research 2022, 9891689 (2022).
Xu, Y. et al. Transcriptional programs controlling perinatal lung maturation. PLoS ONE 7, e37046 (2012).
Swonger, J. M., Liu, J. S., Ivey, M. J. & Tallquist, M. D. Genetic tools for identifying and manipulating fibroblasts in the mouse. Differentiation 92, 66–83 (2016).
Ghasemi, M., Seidkhani, H., Tamimi, F., Rahgozar, M. & Masoudi-Nejad, A. Centrality measures in biological networks. Curr. Bioinformatics 9, 426–441 (2014).
Hermenean, A. et al. Galectin 1—a key player between tissue repair and fibrosis. Int. J. Mol. Sci. 23, 5548 (2022).
Gremlich, S. et al. Tenascin-C inactivation impacts lung structure and function beyond lung development. Sci. Rep. 10, 5118 (2020).
Qiu, X. et al. Reversed graph embedding resolves complex single-cell trajectories. Nat. Methods 14, 979–982 (2017).
Alsafadi, H. N. et al. An ex vivo model to induce early fibrosis-like changes in human precision-cut lung slices. Am. J. Physiol. 312, L896–L902 (2017).
Santoro, A. et al. SERPINE2 inhibits IL-1α-induced MMP-13 expression in human chondrocytes: involvement of ERK/NF-κB/AP-1 pathways. PLoS ONE 10, e0135979 (2015).
Lupsa, N. et al. Skin‐homing CD8+ T cells preferentially express GPI‐anchored peptidase inhibitor 16, an inhibitor of cathepsin K. Eur. J. Immunol. 48, 1944–1957 (2018).
Black, S. et al. CODEX multiplexed tissue imaging with DNA-conjugated antibodies. Nat. Protoc. 16, 3802–3835 (2021).
Wu, X. et al. Regulating the cell shift of endothelial cell-like myofibroblasts in pulmonary fibrosis. Eur. Resp. J. 61, 2201799 (2023).
Habermann, A. C. et al. Single-cell RNA sequencing reveals profibrotic roles of distinct epithelial and mesenchymal lineages in pulmonary fibrosis. Sci. Adv. 6, eaba1972 (2020).
Tsukui, T., Wolters, P. J. & Sheppard, D. Alveolar fibroblast lineage orchestrates lung inflammation and fibrosis. Nature 631, 627–634 (2024).
Buechler, M. B. et al. Cross-tissue organization of the fibroblast lineage. Nature 593, 575–579 (2021).
Liu, X. et al. Multiple fibroblast subtypes contribute to matrix deposition in pulmonary fibrosis. Am. J. Resp. Cell Mol. Biol. 69, 45–56 (2023).
Hallowell, R. W., Amariei, D. & Danoff, S. K. Intravenous immunoglobulin as potential adjunct therapy for interstitial lung disease. Ann. Am. Thorac. Soc. 13, 1682–1688 (2016).
Southam, D. S., Dolovich, M., O’byrne, P. M. & Inman, M. D. Distribution of intranasal instillations in mice: effects of volume, time, body position, and anesthesia. Am. J. Physiol. 282, L833–L839 (2002).
Henderson, W. R. et al. Inhibition of Wnt/β-catenin/CREB binding protein (CBP) signaling reverses pulmonary fibrosis. Proc. Natl Acad. Sci. USA 107, 14309–14314 (2010).
Stuart, T., Srivastava, A., Madad, S., Lareau, C. A. & Satija, R. Single-cell chromatin state analysis with Signac. Nat. Methods 18, 1333–1341 (2021).
Korsunsky, I. et al. Fast, sensitive and accurate integration of single-cell data with Harmony. Nat. Methods 16, 1289–1296 (2019).
Mo, Y. et al. Intratracheal administration of mesenchymal stem cells modulates lung macrophage polarization and exerts anti-asthmatic effects. Sci. Rep. 12, 11728 (2022).
Urbanek, K. et al. Intratracheal administration of mesenchymal stem cells modulates tachykinin system, suppresses airway remodeling and reduces airway hyperresponsiveness in an animal model. PLoS ONE 11, e0158746 (2016).
Govek, K. W. et al. Single-cell transcriptomic analysis of mIHC images via antigen mapping. Sci. Adv. 7, eabc5464 (2021).
Csardi, G. & Nepusz, T. The igraph software package for complex network research. InterJournal 1695, 1–9 (2006).