Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399, 629–655 (2022).
Won, S. Y. et al. Emergence and rapid regional spread of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin. Infect. Dis. 53, 532–540 (2011).
D’Agata, E. M., Habtemariam, D. & Mitchell, S. Multidrug-resistant Gram-negative bacteria: inter- and intradissemination among nursing homes of residents with advanced dementia. Infect. Control Hosp. Epidemiol. 36, 930–935 (2015).
McKinnell, J. A. et al. Prevalence of and factors associated with multidrug resistant organism (MDRO) colonization in 3 nursing homes. Infect. Control Hosp. Epidemiol. 37, 1485–1488 (2016).
Mody, L. et al. Longitudinal assessment of multidrug-resistant organisms in newly admitted nursing facility patients: implications for an evolving population. Clin. Infect. Dis. 67, 837–844 (2018).
Snitkin, E. S. et al. Integrated genomic and interfacility patient-transfer data reveal the transmission pathways of multidrug-resistant Klebsiella pneumoniae in a regional outbreak. Sci. Transl. Med. 9, eaan0093 (2017).
Harrison, E. M. et al. Transmission of methicillin-resistant Staphylococcus aureus in long-term care facilities and their related healthcare networks. Genome Med. 8, 102 (2016).
van den Dool, C., Haenen, A., Leenstra, T. & Wallinga, J. The role of nursing homes in the spread of antimicrobial resistance over the healthcare network. Infect. Control Hosp. Epidemiol. 37, 761–767 (2016).
Haque, M., Sartelli, M., McKimm, J. & Abu Bakar, M. Health care-associated infections—an overview. Infect Drug Resist 11, 2321–2333 (2018).
World Health Organization WHO Bacterial Priority Pathogens List, 2024 (World Health Organization, 2024).
World Health Organization WHO Fungal Priority Pathogens List To Guide Research, Development and Public Health Action (World Health Organization, 2022).
Lapp, Z. et al. Regional spread of blaNDM-1-containing Klebsiella pneumoniae ST147 in post-acute care facilities. Clin. Infect. Dis. 73, 1431–1439 (2021).
Burgess, M. J. et al. Long-term care facilities are reservoirs for antimicrobial-resistant sequence type 131 Escherichia coli. Open Forum Infect. Dis. 2, ofv011 (2015).
Mills, E. G. et al. A one-year genomic investigation of Escherichia coli epidemiology and nosocomial spread at a large US healthcare network. Genome Med. 14, 147 (2022).
Ranjan, A. et al. Comparative genomics of Escherichia coli isolated from skin and soft tissue and other extraintestinal infections. mBio 8, e01070-17 (2017).
Mortensen, E. et al. Multidrug-resistant Acinetobacter baumannii infection, colonization, and transmission related to a long-term care facility providing subacute care. Infect. Control Hosp. Epidemiol. 35, 406–411 (2014).
Pacilli, M. et al. Regional emergence of Candida auris in Chicago and lessons learned from intensive follow-up at 1 ventilator-capable skilled nursing facility. Clin. Infect. Dis. 71, e718–e725 (2020).
Miller, L. G. et al. Decolonization in nursing homes to prevent infection and hospitalization. N. Engl. J. Med. 389, 1766–1777 (2023).
Biran, R. et al. Nationwide outbreak of Candida auris infections driven by COVID-19 hospitalizations, Israel, 2021–2022. Emerg. Infect. Dis. 29, 1297–1301 (2023).
National Center for Emerging and Zoonotic Infectious Diseases (U.S.). Division of Healthcare Quality Promotion. COVID-19: U.S. Impact on Antimicrobial Resistance, Special Report 2022 (Centers for Disease Control and Prevention, 2022).
Lyman, M. et al. Worsening spread of Candida auris in the United States, 2019 to 2021. Ann. Intern. Med. 176, 489–495 (2023).
Sengupta, M., Lendon, J. P., Caffrey, C., Melekin, A. & Singh, P. Post-Acute and Long-Term Care Providers and Services Users in the United States, 2017–2018 (National Center for Health Statistics, 2022).
Snyder, G. M., O’Fallon, E. & D’Agata, E. M. Co-colonization with multiple different species of multidrug-resistant Gram-negative bacteria. Am. J. Infect. Control. 39, 506–510 (2011).
Miller, W. R. & Arias, C. A. ESKAPE pathogens: antimicrobial resistance, epidemiology, clinical impact and therapeutics. Nat. Rev. Microbiol. 22, 598–616 (2024).
Reddy, P. et al. Screening for extended-spectrum β-lactamase-producing Enterobacteriaceae among high-risk patients and rates of subsequent bacteremia. Clin. Infect. Dis. 45, 846–852 (2007).
Willems, R. P. J. et al. Incidence of infection with multidrug-resistant Gram-negative bacteria and vancomycin-resistant enterococci in carriers: a systematic review and meta-regression analysis. Lancet Infect. Dis. 23, 719–731 (2023).
Beezhold, D. W. et al. Skin colonization with vancomycin-resistant enterococci among hospitalized patients with bacteremia. Clin. Infect. Dis. 24, 704–706 (1997).
Bonten, M. J. et al. Epidemiology of colonisation of patients and environment with vancomycin-resistant enterococci. Lancet 348, 1615–1619 (1996).
Jackson, S. S. et al. Bacterial burden is associated with increased transmission to healthcare workers from patients colonized with vancomycin-resistant Enterococcus. Am. J. Infect. Control 47, 13–17 (2019).
Vernon, M. O. et al. Chlorhexidine gluconate to cleanse patients in a medical intensive care unit: the effectiveness of source control to reduce the bioburden of vancomycin-resistant enterococci. Arch. Intern. Med. 166, 306–312 (2006).
Huang, S. S. et al. Targeted versus universal decolonization to prevent ICU infection. N. Engl. J. Med. 368, 2255–2265 (2013).
Li, S. S. et al. Durable coexistence of donor and recipient strains after fecal microbiota transplantation. Science 352, 586–589 (2016).
Siranosian, B. A. et al. Rare transmission of commensal and pathogenic bacteria in the gut microbiome of hospitalized adults. Nat. Commun. 13, 586 (2022).
Ward, D. V. et al. Metagenomic sequencing with strain-level resolution implicates uropathogenic E. coli in necrotizing enterocolitis and mortality in preterm infants. Cell Rep. 14, 2912–2924 (2016).
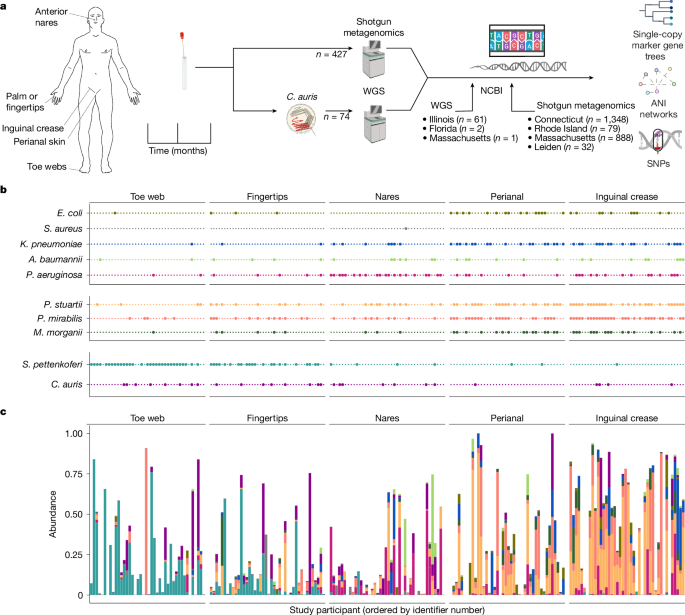
Proctor, D. M. et al. Integrated genomic, epidemiologic investigation of Candida auris skin colonization in a skilled nursing facility. Nat. Med. 27, 1401–1409 (2021).
Trick, W. E. et al. Electronic public health registry of extensively drug-resistant organisms, Illinois, USA. Emerg. Infect. Dis. 21, 1725–1732 (2015).
Peirano, G., Chen, L., Kreiswirth, B. N. & Pitout, J. D. D. Emerging antimicrobial-resistant high-risk Klebsiella pneumoniae clones ST307 and ST147. Antimicrob. Agents Chemother. 64, e01148-20 (2020).
Azar, M. M., Turbett, S. E., Fishman, J. A. & Pierce, V. M. Donor-derived transmission of Candida auris during lung transplantation. Clin. Infect. Dis. 65, 1040–1042 (2017).
Larson, P. J. et al. Associations of the skin, oral and gut microbiome with aging, frailty and infection risk reservoirs in older adults. Nat. Aging 2, 941–955 (2022).
Haran, J. P., Bucci, V., Dutta, P., Ward, D. & McCormick, B. The nursing home elder microbiome stability and associations with age, frailty, nutrition and physical location. J. Med. Microbiol. 67, 40–51 (2018).
Haran, J. P. et al. The high prevalence of Clostridioides difficile among nursing home elders associates with a dysbiotic microbiome. Gut Microbes 13, 1897209 (2021).
Araos, R. et al. Fecal microbiome characteristics and the resistome associated with acquisition of multidrug-resistant organisms among elderly subjects. Front. Microbiol. 10, 2260 (2019).
Ducarmon, Q. R. et al. Microbiota-associated risk factors for asymptomatic gut colonisation with multi-drug-resistant organisms in a Dutch nursing home. Genome Med. 13, 54 (2021).
Saheb Kashaf, S. et al. Staphylococcal diversity in atopic dermatitis from an individual to a global scale. Cell Host Microbe 31, 578–592 (2023).
World Health Organization. Press release: WHO Publishes List of Bacteria For Which New Antibiotics Are Urgently Needed (World Health Organization, 27 February 2017).
Joglekar, P. et al. Integrated genomic and functional analyses of human skin-associated Staphylococcus reveal extensive inter- and intra-species diversity. Proc. Natl Acad. Sci. USA 120, e2310585120 (2023).
Kierzkowska, M., Markowska, K. & Majewska, A. Knowledge, attitude and practice regarding Staphylococcus pettenkoferi. Infect. Dis. Rep. 14, 112–120 (2022).
Lerner, A. et al. Environmental contamination by carbapenem-resistant Enterobacteriaceae. J. Clin. Microbiol. 51, 177–181 (2013).
Sansom, S. E. et al. Rapid environmental contamination with Candida auris and multidrug-resistant bacterial pathogens near colonized patients. Clin. Infect. Dis. 78, 1276–1284 (2024).
Oh, J. et al. Biogeography and individuality shape function in the human skin metagenome. Nature 514, 59–64 (2014).
Martin, M. Cutadapt removes adapter sequences from high-throughput sequencing reads. EMBnet.Journal https://doi.org/10.14806/ej.17.1.200 (2011).
Schmieder, R. & Edwards, R. Quality control and preprocessing of metagenomic datasets. Bioinformatics 27, 863–864 (2011).
Langmead, B., Trapnell, C., Pop, M. & Salzberg, S. L. Ultrafast and memory-efficient alignment of short DNA sequences to the human genome. Genome Biol. 10, R25 (2009).
Bankevich, A. et al. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 19, 455–477 (2012).
Li, D., Liu, C. M., Luo, R., Sadakane, K. & Lam, T. W. MEGAHIT: an ultra-fast single-node solution for large and complex metagenomics assembly via succinct de Bruijn graph. Bioinformatics 31, 1674–1676 (2015).
Uritskiy, G. V., DiRuggiero, J. & Taylor, J. MetaWRAP—a flexible pipeline for genome-resolved metagenomic data analysis. Microbiome 6, 158 (2018).
Orakov, A. et al. GUNC: detection of chimerism and contamination in prokaryotic genomes. Genome Biol. 22, 178 (2021).
Saheb Kashaf, S. et al. Integrating cultivation and metagenomics for a multi-kingdom view of skin microbiome diversity and functions. Nat. Microbiol. 7, 169–179 (2022).
Chklovski, A. et al. CheckM2: a rapid, scalable and accurate tool for assessing microbial genome quality using machine learning. Nat. Methods 20, 1203–1212 (2023).
Parks, D. H., Imelfort, M., Skennerton, C. T., Hugenholtz, P. & Tyson, G. W. CheckM: assessing the quality of microbial genomes recovered from isolates, single cells, and metagenomes. Genome Res. 25, 1043–1055 (2015).
Chaumeil, P. A., Mussig, A. J., Hugenholtz, P. & Parks, D. H. GTDB-Tk: a toolkit to classify genomes with the Genome Taxonomy Database. Bioinformatics 36, 1925–1927 (2019).
Saary, P., Mitchell, A. L. & Finn, R. D. Estimating the quality of eukaryotic genomes recovered from metagenomic analysis with EukCC. Genome Biol. 21, 244 (2020).
Ondov, B. D. et al. Mash: fast genome and metagenome distance estimation using MinHash. Genome Biol. 17, 132 (2016).
Marcais, G. et al. MUMmer4: a fast and versatile genome alignment system. PLoS Comput. Biol. 14, e1005944 (2018).
Gurevich, A., Saveliev, V., Vyahhi, N. & Tesler, G. QUAST: quality assessment tool for genome assemblies. Bioinformatics 29, 1072–1075 (2013).
Ewels, P., Magnusson, M., Lundin, S. & Kaller, M. MultiQC: summarize analysis results for multiple tools and samples in a single report. Bioinformatics 32, 3047–3048 (2016).
Nawrocki, E. P., Kolbe, D. L. & Eddy, S. R. Infernal 1.0: inference of RNA alignments. Bioinformatics 25, 1335–1337 (2009).
Li, H. & Durbin, R. Fast and accurate long-read alignment with Burrows–Wheeler transform. Bioinformatics 26, 589–595 (2010).
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
McMurdie, P. J. & Holmes, S. phyloseq: an R package for reproducible interactive analysis and graphics of microbiome census data. PLoS ONE 8, e61217 (2013).
Wood, D. E., Lu, J. & Langmead, B. Improved metagenomic analysis with Kraken 2. Genome Biol. 20, 257 (2019).
Inouye, M. et al. SRST2: rapid genomic surveillance for public health and hospital microbiology labs. Genome Med. 6, 90 (2014).
Jia, B. et al. CARD 2017: expansion and model-centric curation of the comprehensive antibiotic resistance database. Nucleic Acids Res. 45, D566–D573 (2017).
Olm, M. R., Brown, C. T., Brooks, B. & Banfield, J. F. dRep: a tool for fast and accurate genomic comparisons that enables improved genome recovery from metagenomes through de-replication. ISME J. 11, 2864–2868 (2017).
Jain, C., Rodriguez, R. L., Phillippy, A. M., Konstantinidis, K. T. & Aluru, S. High throughput ANI analysis of 90 K prokaryotic genomes reveals clear species boundaries. Nat. Commun. 9, 5114 (2018).
Achtman, M. et al. Multilocus sequence typing as a replacement for serotyping in Salmonella enterica. PLoS Pathog. 8, e1002776 (2012).
Lee, M. D. GToTree: a user-friendly workflow for phylogenomics. Bioinformatics 35, 4162–4164 (2019).
van Dijk, L. R. et al. StrainGE: a toolkit to track and characterize low-abundance strains in complex microbial communities. Genome Biol. 23, 74 (2022).
Olm, M. R. et al. inStrain profiles population microdiversity from metagenomic data and sensitively detects shared microbial strains. Nat. Biotechnol. 39, 727–736 (2021).
Hyatt, D. et al. Prodigal: prokaryotic gene recognition and translation initiation site identification. BMC Bioinformatics 11, 119 (2010).
Croucher, N. J. et al. Rapid phylogenetic analysis of large samples of recombinant bacterial whole genome sequences using Gubbins. Nucleic Acids Res. 43, e15 (2015).
Zhao, B., Lees, J. A., Wu, H., Yang, C. & Falush, D. Genealogical inference and more flexible sequence clustering using iterative-PopPUNK. Genome Res. 33, 988–998 (2023).
Page, A. J. et al. Roary: rapid large-scale prokaryote pan genome analysis. Bioinformatics 31, 3691–3693 (2015).
Tonkin-Hill, G. et al. Robust analysis of prokaryotic pangenome gene gain and loss rates with Panstripe. Genome Res. 33, 129–140 (2023).
Griffith, D. M., Veech, J. A. & Marsh, C. J. cooccur: probabilistic species co-occurrence analysis in R. J. Stat. Softw. Code Snip. 69, 1–17 (2016).
Reichel, M., Heisig, P. & Kampf, G. Pitfalls in efficacy testing—how important is the validation of neutralization of chlorhexidine digluconate? Ann. Clin. Microbiol. Antimicrob. 7, 20 (2008).
Welsh, R. M. et al. Survival, persistence, and isolation of the emerging multidrug-resistant pathogenic yeast Candida auris on a plastic health care surface. J. Clin. Microbiol. 55, 2996–3005 (2017).
Koren, S. et al. Canu: scalable and accurate long-read assembly via adaptive k-mer weighting and repeat separation. Genome Res. 27, 722–736 (2017).
Vaser, R., Sovic, I., Nagarajan, N. & Sikic, M. Fast and accurate de novo genome assembly from long uncorrected reads. Genome Res. 27, 737–746 (2017).
Walker, B. J. et al. Pilon: an integrated tool for comprehensive microbial variant detection and genome assembly improvement. PLoS ONE 9, e112963 (2014).
Tarailo-Graovac, M. & Chen, N. Using RepeatMasker to identify repetitive elements in genomic sequences. Curr. Protoc. Bioinformatics Ch 4, 4.10.1–14.10.14 (2009).
Garrison, E. & Marth, G. Haplotype-based variant detection from short-read sequencing. Preprint at https://arxiv.org/abs/1207.3907 (2021).
DePristo, M. A. et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat. Genet. 43, 491–498 (2011).
Nguyen, L. T., Schmidt, H. A., von Haeseler, A. & Minh, B. Q. IQ-TREE: a fast and effective stochastic algorithm for estimating maximum-likelihood phylogenies. Mol. Biol. Evol. 32, 268–274 (2015).
Knaus, B. J. & Grunwald, N. J. vcfr: a package to manipulate and visualize variant call format data in R. Mol. Ecol. Resour. 17, 44–53 (2017).
Le Bastard, Q. et al. Gut microbiome signatures of nursing home residents carrying Enterobacteria producing extended-spectrum β-lactamases. Antimicrob. Resist. Infect. Control 9, 107 (2020).