James Collins, Andrés Cubillos-Ruiz and Raphaël Gayet co-founded the biotechnology company Florey Biosciences.Credit:
Andrés Cubillos-Ruiz’s wife was four months pregnant when she received a course of antibiotics to prevent invasive bacteria from taking up residence in her gums, following a routine dental procedure.
Nature Outlook: The human microbiome
But the bacteria-killing effects of these drugs weren’t confined to her mouth. Like most systemic antibiotics, they also upended the fragile equilibrium of beneficial microorganisms living in the gut — and given the link between maternal gut health and fetal development, Cubillos-Ruiz worried that the antibiotic exposure might be compromising the health of their unborn daughter.
It is a well-known concern: antibiotics are essential for combating dangerous bacterial infections, but they do not discriminate between harmful and beneficial microbes. Gut microbial communities are often knocked off-kilter, and it can take months for them to fully recover. Until they do, people are more vulnerable to opportunistic infections and to a range of immune, metabolic and cognitive complications.
“Deploying an antibiotic is not a benign act,” says Gautam Dantas, a microbial genomics researcher at the Washington University School of Medicine in St. Louis, Missouri. The drugs often cause “collateral damage”, he explains, disrupting microbial ecosystems in ways that can have long-lasting health effects.
Researchers have tried to remedy the problem with compounds that selectively neutralize antibiotics in the gut without affecting the rest of the body, but these efforts have met with limited success. Faced with a lack of a viable solution for his wife, Cubillos-Ruiz, a microbiologist, took it upon himself to confront the issue head-on.
Working in the laboratory of synthetic biologist James Collins at the Massachusetts Institute of Technology (MIT) in Cambridge and the nearby Wyss Institute in Boston, Massachusetts. Cubillos-Ruiz took a bacterium commonly found in fermented foods and engineered it to safely break down a class of antibiotics called β-lactams. These bacteria-killing medications include amoxicillin — the drug that Cubillos-Ruiz’s wife had taken after her dental surgery.
Cubillos-Ruiz and Collins endowed their engineered microbe with the ability to produce a β-lactamase enzyme that degrades amoxicillin. In experiments with mice, this living biotherapeutic released its antibiotic-neutralizing payload directly into the gut, shielding the microbes within from the antibiotic’s effects. But crucially, the antibiotic retained its infection-fighting capabilities elsewhere in the body1.
Recognizing the potential of their discovery and the widespread clinical need — millions of prescriptions for antibiotics are issued daily around the globe — Cubillos-Ruiz and Collins established a company to bring their gut-defending innovation to people. In October 2024, they and synthetic biologist Raphaël Gayet launched Florey Biosciences, named in honour of Howard Florey, the Australian pharmacologist who shared the 1945 Nobel Prize in Medicine or Physiology for the development of penicillin.
Other companies sell probiotics to offset the damage caused by antibiotics. But studies show that these supplements — typically a cocktail of bacteria found in a healthy gut — do not restore microbial diversity effectively, and might even delay the gut’s natural recovery process2. Although there have been other efforts to develop pharmaceuticals that prevent beneficial microbes from being depleted in the first place, none has yet successfully navigated the regulatory challenges needed to bring such a product to market.
With its engineered, gut-defending microbe, Florey Biosciences in Boston says it can do better — and in so doing, shift the model of antibiotic therapy towards approaches that eliminate harmful infections without disrupting the delicate balance of the healthy gut microbiome.
Guardians of gut health
The failures of several once-promising approaches to reduce the collateral damage of antibiotics has often stemmed from commercial and regulatory problems, rather than biological hurdles.
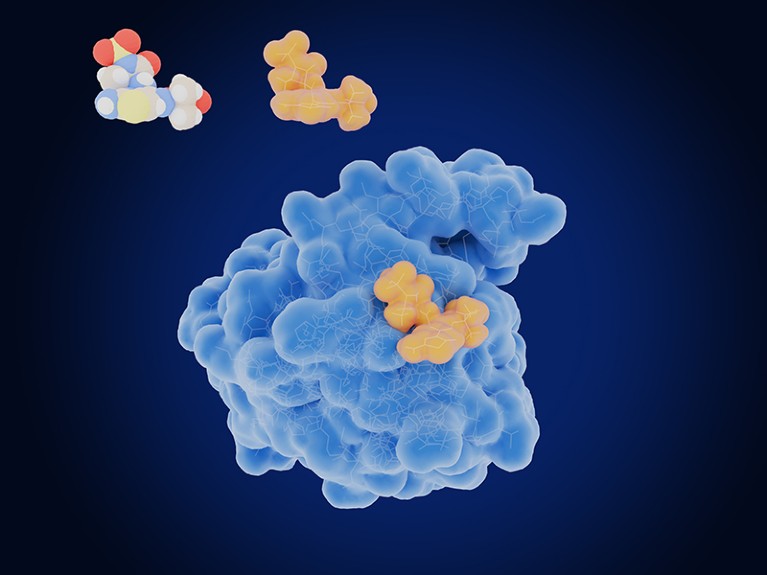
The enzyme β-lactamase (blue) can break down some antibiotics.Credit: JUAN GAERTNER/SPL
Consider, for example, DAV132: a preparation of activated charcoal designed to bind to and neutralize antibiotics in the colon. Trials performed in the late 2010s, both in healthy volunteers3 and in people in hospital4, found that taking the drug alongside antibiotics helped to protect the gut microbiome from disturbances, without compromising the effectiveness of the antibiotics in the bloodstream.
Maria Vehreschild, an infectious-disease specialist at University Hospital Frankfurt in Germany, saw those early results as clear evidence that DAV132 was performing as intended. “I’m convinced that it works,” she says.
However, protection of microbial diversity is not recognized as a health benefit that is sufficient for regulatory authorization. To meet approval standards, Da Volterra, the Paris-based company which was behind DAV132, would have needed to prove that the companion drug could prevent life-threatening infections in people who were taking antibiotics.
History suggested that this would be challenging. Years earlier, a company called Synthetic Biologics (now known as Theriva Biologics) in Rockville, Maryland, had been developing a purified formulation of β-lactamase — no engineered microbe required. In 2015, the company initiated a placebo-controlled trial involving hundreds of people who were hospitalized for pneumonia, all of whom were treated with a powerful broad-spectrum β-lactam antibiotic.
Although these antibiotics are effective against respiratory infections, the treatment leaves people vulnerable to Clostridioides difficile, a potentially deadly pathogen that causes severe diarrhoea and colitis. The study indicated that those who received the gut-protecting β-lactamase, called SYN-004, alongside the antibiotic, had reduced incidence of C. difficile infection5.
However, the overall number of infections seen in the study was low — only 7 of 206 people in the placebo group of the trial contracted C. difficile, and 2 of 207 receiving active treatment. With such a low incidence of documented infections, Synthetic Biologics estimated that it would need a further US$80 million for a larger trial to confirm the benefits of SYN-004 for gut health, according to Vince Wacher, head of product development.
No investors wanted to take the risk. “That’s the challenge with prevention,” Wacher says. “It’s something that is difficult to sell.”
Proactive prevention
With limited financial resources, Synthetic Biologics pivoted its focus to an entirely different area of drug development — cancer-killing virus therapies.
SYN-004 was not abandoned altogether, however. The company opted to give the β-lactamase drug one more shot, but with a narrowed target to make the clinical testing more feasible: people with blood cancer who were receiving stem-cell transplants from donor bone marrow.
Antibiotics are a crucial component of the care regimen for this group, but they can trigger immune-related complications — particularly graft-versus-host disease, which affects up to half of these individuals. Compared with the company’s initial goal, the market opportunity is significantly smaller. Only around 40,000 people worldwide undergo this type of transplant therapy each year, compared with millions who receive β-lactam antibiotics for other reasons every day. Early testing of SYN-004 for this specialized indication is ongoing.
Hidden players: the bacteria-killing viruses of the gut microbiome
When developing DAV132, Da Volterra tried to split the difference, aiming to balance broad patient inclusion with a focus on those most susceptible to complications from antibiotic-induced gut disturbances. Its pivotal trial would also be in people with blood cancer who were taking antibiotics, but the study would draw from a much larger population: people undergoing intensive chemotherapy, around 10–20% of whom develop C. difficile infections.
In 2021, a global trial kicked off for DAV132, with the goal of enrolling 900 participants. However, the company encountered difficulties with recruitment, compliance and retention. A year in, only 73 people had signed up, and more than half of these people dropped out fairly quickly. The complex medical needs and short survival horizons of the cohort made it “an exceptionally difficult trial population”, Vehreschild and her fellow study authors concluded6. Da Volterra terminated the trial early and ultimately declared bankruptcy, relegating DAV132 to the annals of pharmaceutical history.
Looking to avoid a similar fate, Florey Biosciences plans to advance its engineered microbe as a ‘medical food’ — a regulatory classification that could streamline its path to market and substantially reduce development costs. That is because medical foods — defined as specially formulated foodstuffs administered into the digestive system under active medical supervision — need only to comply with safety standards and demonstrate suitability for managing specific health conditions. They are exempt from the extensive clinical trials required for pharmaceuticals.
Safety features
Florey Biosciences has also implemented a few synthetic design enhancements to strengthen its chances of achieving therapeutic impact. The company’s lead product, named FLR-101, is now built around a genetically modified strain of Saccharomyces boulardii, a species closely related to baker’s yeast (Saccharomyces cerevisiae) that is already sold in its natural form as a probiotic to treat and prevent digestion problems.
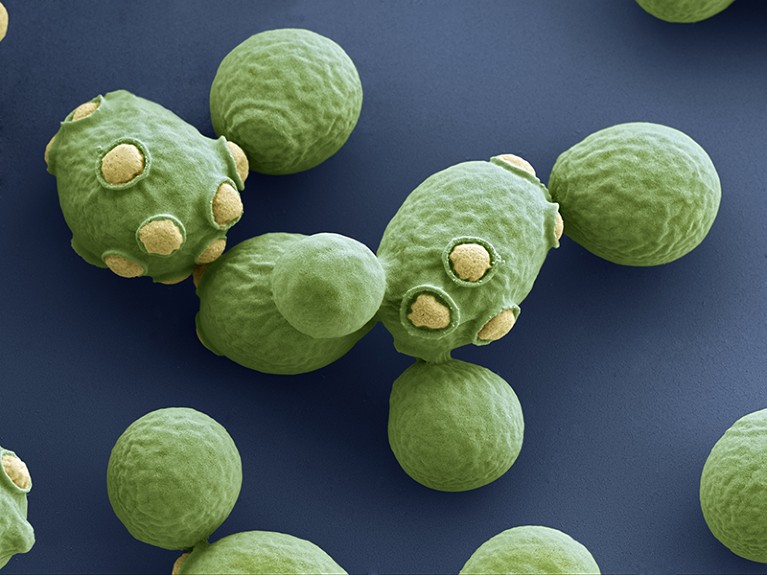
Baker’s yeast (Saccharomyces cerevisiae) is sold as a probiotic to treat digestion problems.Credit: EYE OF SCIENCE/SPL
According to Cubillos-Ruiz (who is now chief executive of Florey Biosciences), this switch from a bacterium to a yeast was made for two reasons: to maximize how much of the β-lactamase enzyme is expressed, and to ensure that the drug-degrading properties of the designer microbe do not spread to the broader population of gut bacteria.
Johann Pitout, a medical microbiologist at the University of Calgary’s Cummings School of Medicine in Canada, warns of the risk that engineered traits could be transferred to other microbes, potentially fuelling widespread antibiotic resistance. “It’s a very dangerous game,” he says.
To mitigate this risk, Cubillos-Ruiz and his colleagues, in a proof-of-concept mouse study, split the engineered β-lactamase expression system into two components. This means that even if gene transfer were to occur between microbes it would be significantly harder for the recipients to acquire the complete functionality. “I must say, that’s very impressive,” Pitout says.
By opting for yeast instead of a bacterium, Florey Biosciences is adding an extra layer of safety. The transfer of genetic material between different domains of life is exceedingly rare, so these precautions should ensure that FLR-101 does not jeopardize the effectiveness of current antibiotics, while still providing benefit for users. “This is not just for the individual,” Cubillos-Ruiz says. “This is for public health as well.”
Cubillos-Ruiz is confident that FLR-101, when paired with antibiotics, will lead to less microbiome damage than would treatment with antibiotics alone — a suggestion he plans to validate in clinical trials. If successful, the company could then market the engineered yeast as a targeted solution for managing gut dysfunction, distinguishing it from other probiotics on the pharmacy shelf. Cubillos-Ruiz hopes to launch the product commercially by 2027.
Fortifying flora
Some research indicates that lower-tech dietary interventions could be just as effective at protecting gut microbes from the effects of antibiotics.
For example, diets high in fat and low in fibre have been linked to greater disturbances of the gut microbiome in mouse models of antibiotic-induced C. difficile infection7 — a finding that prompted study author Catherine Lozupone to initiate a clinical trial of a high-fibre diet in people with leukaemia or lymphoma. “Fibre really shores up your microbiome in the context of antibiotics,” says Lozupone, a microbial ecologist at the University of Colorado Anschutz Medical Campus in Aurora.
Another study, in mice, sheds light on the potential mechanistic basis for fibre’s beneficial effects. Microbial biochemist Peter Belenky and his team at Brown University in Providence, Rhode Island, demonstrated that these nutritionally advantageous carbohydrates can alter the metabolic activity of intestinal microbes, effectively shielding them from the onslaught of antibiotics8. “It puts them into a kind of suspended animation,” Belenky explains.
Collins, for his part, is hedging his bets when it comes to the challenge of combating antibiotic-induced gut dysfunction. As well as his efforts with Florey Biosciences to disarm drugs locally in the gut with engineered yeast, he is also using artificial-intelligence technology to search for antibiotics that work selectively against pathogens without damaging beneficial microbes elsewhere in the body.
In 2023, Collins and Jonathan Stokes, a microbial chemical biologist at McMaster University in Hamilton, Canada, identified one such compound with narrow-spectrum activity against Acinetobacter baumannii, a common cause of hospital-acquired infections9. In cell-culture experiments, this compound had minimal impact on beneficial bacteria in the gut and on the skin, whereas commonly prescribed broad-spectrum agents such as ampicillin and ciprofloxacin wiped out these microbes.
Other teams are using the genome-editing CRISPR–Cas system to engineer bacteria-killing viruses, known as bacteriophages, to target and eradicate specific bacterial species or strains. And some companies, including Seres Therapeutics and Vedanta Biosciences, both based in Cambridge, Massachusetts, are crafting consortia of cultivated bacterial strains that can minimize the chance of harmful pathogens colonizing the gut after antibiotic treatment.
In comparison to food-grade products, these types of pharmaceutical or live biotherapeutic need to go through a longer and more complex regulatory process before they can enter the market. Nonetheless, the progression of multiple candidates through diverse regulatory pathways is likely to boost the odds of a viable solution emerging.
After years of intermittent progress, the rising awareness of the microbiome’s importance to overall health is now driving a wave of innovation in the antibiotic-protection space. “People are waking up to the need to better manage our microbiome in the face of antibiotic treatment,” Collins says. This awakening might just be the push the field has been waiting for.