Current methods for diagnosing obesity don’t capture the complexity of the condition, say researchers.Credit: BSIP/Universal Images Group via Getty
Amid the rising buzz around Ozempic and similar weight-loss drugs, a group of 58 researchers is challenging the way obesity is defined and diagnosed, arguing that current methods fail to capture the complexity of the condition. They offer a more nuanced approach.
The group’s revised definition, published in The Lancet Diabetes & Endocrinology1 on 14 January, focuses on how excess body fat, a measure called adiposity, affects the body, rather than relying only on body mass index (BMI), which links a person’s weight to their height. They propose two categories: preclinical obesity, when a person has extra body fat but their organs work normally, and clinical obesity, when excess fat harms the body’s organs and tissues.
Why BMI is flawed — and how to redefine obesity
This shift could improve clinical care, public-health policies and societal attitudes toward obesity, says Elisabeth van Rossum, an endocrinologist at the Erasmus University Medical Center Rotterdam in the Netherlands.
“Now the idea is, eat less, move more, and you’ll lose weight,” says van Rossum, who wasn’t involved in the work. Although a healthy lifestyle is important, she adds, “if it would be so simple, we wouldn’t have an epidemic, and this paper is an excellent contribution to the discussion about the complexity of obesity”.
Global problem
More than 1 billion people worldwide live with obesity, and the condition is linked to about 5 million deaths every year2 from disorders such as diabetes and cardiovascular disease.
Because it is easy to measure and compare, BMI has long been used as a tool to diagnose obesity. But it doesn’t offer a full picture of a person’s health, because it doesn’t account for differences in body composition, such as muscle versus fat.
How ‘miracle’ weight-loss drugs will change the world
For people of European descent, obesity is typically defined by a BMI of 30 or higher, which correlates with a high level of body fat. However, a muscular athlete might be labelled obese on the basis of BMI, whereas someone with a ‘normal’ BMI might have excess fat that increases their risk of heart problems or other serious health issues, says Francesco Rubino, a bariatric surgeon at King’s College London, who led the group proposing the new approach.
Conventional methods lead to unnecessary treatment for some people while missing others who need help, he says. To address this, Rubino and his colleagues propose a system for diagnosing obesity that goes beyond BMI, combining it with other methods such as measuring waist circumference, which is a proxy for adiposity, or body scans using low-level X-rays, which can directly measure fat mass.
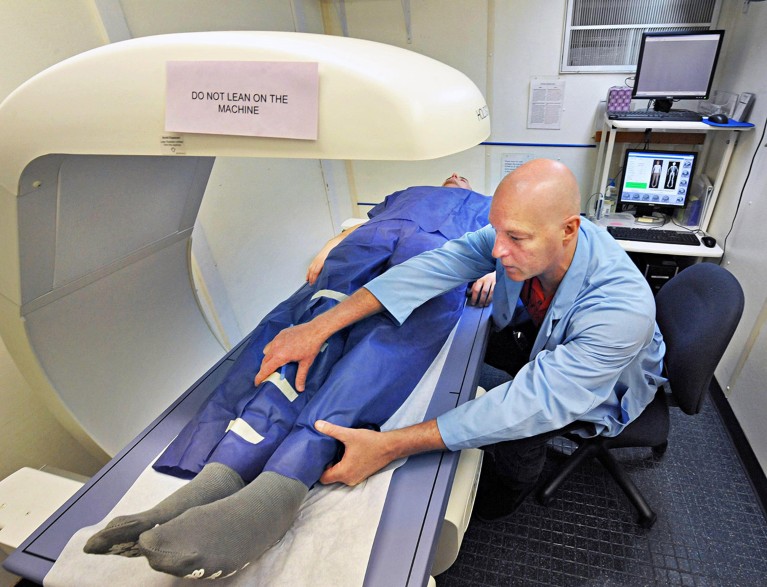
A DEXA body scan, which uses low-dose X-rays, can measure body fat, but it might be impractical or expensive for routine diagnoses of obesity.Credit: John Carl D’Annibale/Albany Times Union via Getty
Although there isn’t a fixed threshold for obesity, body fat is typically considered to be in excess when it is above 25% in men and 30–38% in women. Because measuring adiposity directly might be impractical or costly, alternative health markers such as waist size, waist-to-hip ratio or waist-to-height ratio are important, the researchers say. However, they add, it’s safe to assume that a person with a BMI above 40 has high body fat.
Diagnosing obesity should also consider the results of standard laboratory tests, medical history, and information on daily activities to assess how excess body fat might affect a person’s health, says study co-author Robert Eckel, an endocrinologist at the University of Colorado Anschutz Medical Campus in Aurora. “These are objective diagnostic criteria, they’re standardized across global health systems,” he says.
How rival weight-loss drugs fare at treating obesity, diabetes and more
Personalized assessments that consider age, gender and ethnicity are equally important, because certain groups might face health risks at lower BMI thresholds than others, says study co-author Louise Baur, a paediatrician at the University of Sydney, Australia.