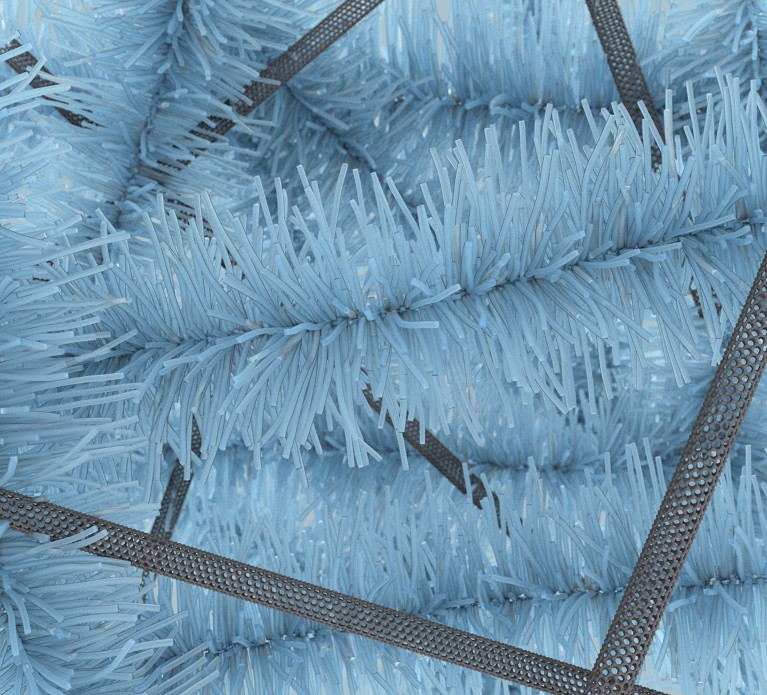
A rendering of a bottlebrush elastomer and carbon-nanotube composite that researchers believe has potential use as a brain electrode.Credit: Xu, P. et al. Nature Commun. 14, 623 (2023)/CC BY 4.0
When Shuai Xu set out to create a wearable biosensor to monitor the vital signs of premature infants and newborns, he faced a major challenge: the skin of these children is so delicate that the adhesive used to attach a sensor could damage it, potentially leading to infection. The stiff device pulling against the skin as the baby moved, and the wires that might pull it in a different direction, added to the problem. The solution was to build a sensor that was soft and stretchable, with flexible circuit boards and thin, 50-millimetre wires, a huge change from the rigid devices that had long been a mainstay of this type of engineering. It was encased in a bendable silicone, transmitted its readings via Bluetooth, and was stuck to the body using a hydrogel, a polymer-based substance made mostly of water. Xu, a dermatologist, helped develop the device as a postdoctoral researcher in the laboratory of John Rogers, an engineer and materials scientist at Northwestern University in Evanston, Illinois, a pioneer in soft materials.
Xu went on to become a founder and chief executive of Sibel Health in Chicago, Illinois, a medical device company that won Nature’s Spinoff Prize in 2020 and sells wearable sensors for monitoring patients. Xu’s challenges are common among researchers trying to develop biosensors and the materials that go into creating them. The devices must be small and lightweight, and must attach to the body with minimum irritation. In some cases, they require long-lasting batteries and circuitry that can handle a growing suite of artificial-intelligence algorithms that make sense of the data they collect.
Nature Index 2024 Materials science
According to one estimate, the global market for health sensors was worth an estimated US$42.6 billion in 2023 and expected to grow to US$142.2 billion by 2030. The wrist-worn or finger-worn devices that were designed to count steps can now measure heartbeat and blood-oxygen levels, and they’ve been joined by patches that allow diabetics to perform continuous monitoring of their glucose levels.
“That’s nothing to sneeze at,” Xu says. “But there are so many other things that are out there, biochemical and biophysical, that we still can’t do in a practical, continuous way.” Figuring out how to measure a variety of physical and chemical signals cheaply and non-invasively could provide diagnostic information that could reshape medicine. And this might go beyond sensors that take mechanical measurements, such as heart rate. Researchers are also working on chemical sensors that can detect biomarkers in blood, sweat and tears, as well as in fluids that surround cells.
Aida Ebrahimi, a biosensor engineer at Pennsylvania State University in State College, is working on materials that can detect neurotransmitters in saliva or urine such as dopamine, serotonin, adrenaline and noradrenaline, which change in people with diseases such as Parkinson’s or Alzheimer’s. She’s focused on 2D materials, which are only one atomic layer thick, such as molybdenum disulfide. With a material in which, effectively, the “whole thing is surface, you are going to get high sensitivity in the ability to detect a very low concentration of biomolecules”, says Ebrahimi. The material properties of such atomically thin films are also sensitive to surface modification. For example, attaching molecules of manganese gives the material an affinity for dopamine, creating an ultrasensitive detector1.

A soft and stretchable sensor was developed for a newborn’s sensitive skin.Credit: Northwestern University
Similar materials with different molecules attached could be used as sensors for other chemicals that can provide information about health, says Ebrahimi. Her team built a prototype of the sensor in 2020 that they showed could measure dopamine1, but building it and validating it for use could be several years off.
One measuring challenge is that a lot of signalling, particularly in the brain, is performed by the movement of ions, whereas most monitoring equipment is designed to detect electrical currents carried by the flow of electrons. Sahika Inal, a bioengineer at KAUST in Thuwal, Saudi Arabia, is using organic electrochemical transistors (OECTs)2, devices that can detect signals from biomolecules, cells and lipid layers and turn them into readings that can be measured by electronic equipment. OECTs can be built using organic mixed ionic–electronic conductors (OMIECs), which have been the focus of much interest in the past few years. OMIECs are polymers that both ions and electrons can flow across easily. When part of the transistor experiences a small change in a property it is measuring, the OMIEC amplifies that signal. Because it’s an organic polymer, the material is much more compatible with the wet environment of the body than a standard electronic transistor, which has to be encapsulated to protect it from fluids. As a result, electronics can be developed “that can be integrated directly with the biological system,” Inal says.
OECT’s could be printed directly on the skin’s surface to detect biological signals, for instance, or built on top of threads of fabric to create biosensing garments and wraps that could survive washing. They also have the potential to replace the stiff electrodes used in brain implants to control prosthetic devices and monitor electrical activity in seizure patients. Their flexibility and biocompatibility might cause less irritation to brain tissue, which can render the electrodes less sensitive.
At the University of Toronto, mechanical engineer, Xinyu Liu, and chemical engineer, Helen Tran, have developed another material with the softness and flexibility to be used as a brain electrode3. Dubbed the bottlebrush elastomer, their rubber-like substance is made from a molecule that has a long, stiff spine, which maintains its structure, surrounded by short, flexible bristles, for softness. To give the material electrical conductivity, Liu and Tran add a filler — either carbon nanotubes or a mixture of silver flakes and eutectic gallium indium, a semiconductor in liquid form. They worry, though, that the filler could leech out and have toxic effects, so they’d like to eliminate it. “Ultimately, we would like to design a polymer that is soft and electron-conducting,” Tran says. “These demands are often at odds.”
Liu’s lab is also working on wearable sensors. One, based on a hydrogel, is designed to conform to the skin and measure strain when a body part, a knee, for example — is bent4. Such a device could be useful in monitoring an athlete’s performance or assessing arthritis.
Another sensor they are developing places nanowires of zinc oxide on a cotton thread to create electronic textiles that can measure substances such as lactate and sodium in sweat. The material could be woven into a shirt or a sweatband to monitor an athlete’s health5.
Xu sees a lot of opportunities for new biosensors. “AI is generating new algorithms,” he says, that can then be integrated into sensors to learn from, and react, to measurements they’re recording. That would require developing processors that can work with the limited power available in a sensor. Better batteries might help, as would alternatives such as harvesting power from movement or body heat, he says. Devices that can combine readings — glucose levels with heart rate, for instance — could be transformative, he says. He would also like to be able to detect stress hormones that could be used to monitor fatigue, or drug metabolites to check patients have taken medications.
Biosensors have the potential to collect a lot of useful information, and to do it in everyday settings that might give a more realistic picture of health than a one-time doctor’s test. “Whether you’re ill or not”, says Xu, people do not spend most of their time in a clinic or hospital. The ability to track health “and use the technology yourself, I think is really important”.



