Scientists have developed a blood test that uses biomarkers to help diagnose bipolar disorder.Credit: John Thys/Reporters/Science Photo Library
A first-of-its-kind blood test that uses biomarkers to distinguish bipolar disorder from depression could slash the time it takes to get an accurate diagnosis from years to weeks, according to the company that developed the test — but some scientists have raised concerns about its validity.
The test uses biomarkers related to RNA editing to diagnose the condition and has been available in France since March and in Italy since October 2023, having been granted regulatory approval in both countries.
Blood test uses ‘protein clock’ to predict risk of Alzheimer’s and other diseases
However, some researchers are concerned about the small size of the trials the test is based on and the lack of independent verification of the studies. The test’s developer, the French start-up Alcediag in Montpellier, says that its trials are valid and reproducible.
The row highlights a wider discussion about the potential of biomarkers — biological characteristics that can indicate a particular medical state — to enable earlier diagnosis and more personalized treatments for psychiatric disorders.
“There is a role for investigating biomarkers,” says Suresh Sundram, a psychiatrist at Monash University in Melbourne, Australia. “But it is a very fraught area.”
Slow diagnosis
Bipolar disorder, a spectrum of conditions characterized by mood swings that alternate between mania and depression, is difficult to diagnose. About 40 million people globally live with the illness, and the diagnostic process, which often involves multiple sessions with a psychiatrist, takes an average of seven to ten years, during which time people are often misdiagnosed with conditions such as depression and given inappropriate or ineffective treatments.
Alcediag hopes to alter this grim landscape. The company says its €900 (US$980) blood test, EDIT-B, can help to distinguish bipolar disorder from depression using biomarkers. EDIT-B differentiates between the two by measuring subtle differences in RNA editing — a regulatory process that alters various cellular mechanisms, including the expression of genes, which in turn affects neurological functioning.
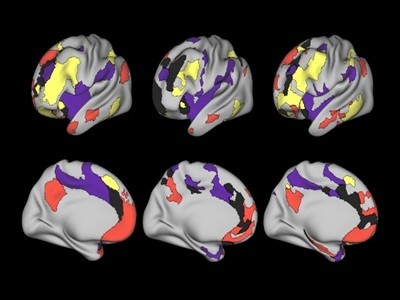
Found: a brain-wiring pattern linked to depression
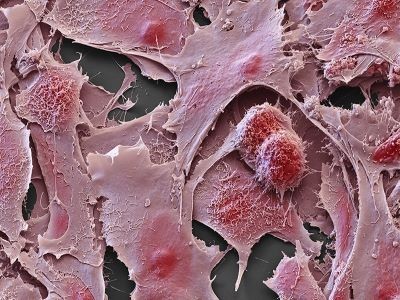
Several studies have suggested that differences in RNA editing could play a part in autoimmune diseases and cancer, as well as in psychiatric conditions. In preliminary research, scientists at Alcediag identified distinct patterns of RNA editing affecting eight genes that seem to differ between healthy people and those experiencing depression. Among the depressed patients, six of these genes also show variations that distinguish people with depression from those with bipolar disorder. These differences produce a unique combination — or signature — of biomarkers that the company says it discovered using an artificial intelligence (AI) algorithm it developed.
“We have a signature for those with depression, a signature for the controls, and … one for bipolar,” says Dinah Weissmann, co-founder and chief scientific officer of Alcediag. In a 2022 study involving 410 participants, the algorithm distinguished between the 160 people with depression and the 95 individuals with bipolar disorder with high accuracy1.
About 80 people have used EDIT-B since its commercialization in France and Italy, says Weissmann, and feedback has been positive so far. She cites the anecdotal report of a person who, after receiving a positive test result, said they changed to more effective medication. “The patient wrote to their doctor: ‘It’s great, I’m back on my feet. I’m living normally again,’” says Weissmann.
Potential risks
For many people with bipolar disorder, a faster, more precise diagnosis would allow them to access “the right medication, at the right time”, says Marion Leboyer, a psychiatrist and executive director of the FondaMental Foundation, a research organisation based near Paris.
On the other hand, if a blood test gives an incorrect result, there is a risk that disorders could be misdiagnosed or overlooked, says Boris Chaumette, a psychiatrist at the French National Institute of Health and Medical Research in Paris.
There is no indication that an EDIT-B result has led to an incorrect diagnosis. But Chaumette and others are concerned about some of the methodology of studies used to demonstrate the EDIT-B test’s effectiveness. He points to “inherent limits” to the 2022 study with 410 participants. “You take a data set with many variables and not many patients, and you ask an algorithm to classify people. It will inevitably find things that classify them, it will inevitably identify commonalities,” he says. “In fact, what you observe could be the effect of treatments.”
Simple blood test detects eight different kinds of cancer
He adds that, apart from the control group, every person involved in Alcediag’s studies was taking medication (as is often the case with psychiatric research). These drugs could affect the levels of some biomarkers, says Sundram, “so the algorithm could pick up the effect of the medicine”.
Weissmann says that the study participants with bipolar disorder and those with depression were taking a range of different medications, so if the algorithm was distinguishing people on the basis of their treatments, it would have classified them according to therapeutic classes. Stable patients — those who had a diagnosis but were not experiencing symptoms at the time of the study — also had a different biomarker signature from the control group, she adds, indicating that their medication suppressed symptoms without affecting markers of the underlying illness. She says that Alcediag’s studies have involved hundreds of participants, and that the company is conducting a new clinical trial with 436 patients; they expect to publish the results next year.
Replication questions
Certain aspects of Alcediag’s studies make it difficult for independent researchers to verify the work, says Chaumette. The algorithm and its underlying code haven’t been shared, and follow-up studies run after the initial 2022 trial have used slightly different versions of the test. In a study the firm published this year, for example, it had removed one biomarker from the initial combination and added three new ones2.
This issue led the French National Authority for Health (HAS), an independent body that assesses health products, to reject Alcediag’s application for people taking the test to be reimbursed by the French health authorities. “There were variations in performance among the three versions, and we lacked the rationale to explain why this version was chosen and not another,” says Cédric Carbonneil, who heads the HAS department responsible for assessing new medical devices and procedures. It is not unusual for companies at early stages of development to initially have their applications denied, and the HAS expects Alcediag to reapply, he adds. Alcediag says that it made changes to the biomarkers to improve the test’s performance, and that it hasn’t shared the algorithm for commercial reasons.
Chaumette says he would have liked to see larger studies backing up the test before it was rolled out to patients, and he hopes Alcediag will make its technology available to independent groups to allow them to replicate the findings. “If you commercialize it rapidly and patent everything without sharing anything, then it becomes opaque.”