
Blood tests could make detecting Alzheimer’s disease easier.Credit: Andrew Brookes/Getty
In 2018, the people around Daryl Ditz started to see signs that something wasn’t quite right. “My work colleagues noticed I was kind of slipping with the computer stuff — messing up a little bit, putting files in the wrong place,” he says. “My wife noticed things around the house. I’d put the keys in the wrong place, that kind of thing.”
In 2021, at the age of 60, he was diagnosed with early-onset Alzheimer’s disease. It had been a struggle to get from a suspicion that he might be ill to an actual diagnosis. That was partly owing to disruptions to the health-care system, and to life in general, during the COVID-19 pandemic. But even with the doggedness of his wife, Nimmi, and family friends, one of whom is a neurologist, who knew their way around health-care systems, it took several months from his first appointment to having a brain scan that provided a definitive answer.
That’s why he was happy to hear the news earlier this year about blood tests that can help to diagnose the disease so that people can receive treatment. “Once people do get the clue or the worry, the best thing they could do is try to find out. So easy, cheap, reliable tests help somebody quickly figure out — is this a problem?” says Ditz in Washington DC, who used to work in environmental policy and is now retired.
Keep your head
Alzheimer’s was first defined in 1906, and for many decades, it was diagnosed by assessing symptoms. The only way to identify it with certainty was through an autopsy after the person had died. In the early 2000s, new methods emerged. Tests of cerebrospinal fluid (CSF) could measure levels of amyloid-β — a peptide that forms destructive plaques in the brains of people with Alzheimer’s — and tau, a protein that accumulates into tangles inside neurons. Positron emission tomography (PET) scans use radioactive tracers to image the plaques and the tangles, and the first agent for highlighting tau pathology was approved by the US Food and Drug Administration (FDA) in 2020.
Part of Nature Outlook: Medical diagnostics
But both of these methods have serious drawbacks. A lumbar puncture is required to collect CSF. And PET scans, in addition to the risks associated with injecting radioactive material, are expensive and not readily available. Even in a densely populated city such as Washington DC, it took Ditz a while to get one; in less populous areas, hospitals offering the service can be hard to find.
The emergence of a test that can measure the same proteins in blood could provide an easier, faster diagnosis for people in a less invasive way, with a simple blood sample at a physician’s surgery. The advent of such tests paves the way to access to newly approved treatments and could lead the way to even earlier diagnosis. The hope is that earlier intervention could stave off dementia before it disrupts people’s lives.
“It’s a really exciting development that we have blood tests for Alzheimer’s,” says Stephen Salloway, a neurologist at Brown University in Providence, Rhode Island, who also directs the Memory and Aging Program at Butler Hospital, which is affiliated with Brown. Salloway notes that no test has yet received FDA approval, although several have been cleared under rules from the US Centers for Medicare and Medicaid Services that certify the quality of laboratory tests and can be ordered by physicians. “I don’t think FDA approval is that far off,” he says. “It’ll come within the next 12 months for sure.”
Several such tests could win approval. For example, Fujirebio, a Tokyo-based biotechnology company, has developed an amyloid-β plasma test that is currently designated for research use only. And the company announced at the end of July that it was teaming up with Biogen in Cambridge, Massachusetts, and Beckman Coulter in Brea, California, to develop a blood test for biomarkers of tau pathology that could be used for diagnosis.
Detecting Alzheimer’s wouldn’t mean much if nothing can be done about it, but the FDA has now granted full approval to two drugs for treatment of early-stage disease. Lecanemab, approved in July 2023, and donanemab, approved in July 2024, are both monoclonal antibodies that reduce amyloid-β plaques and slow cognitive decline by 25–35%. Although other drugs treat some of the symptoms, the monoclonal antibodies are the first that aim to stop its progression by shrinking the plaques. The result, says Salloway, is that people stay in the early, mild stage of Alzheimer’s longer. “That’s what people want,” he says. But because the drugs work by degrading the plaque, under FDA rules they cannot be prescribed until the existence of the plaques has been confirmed.
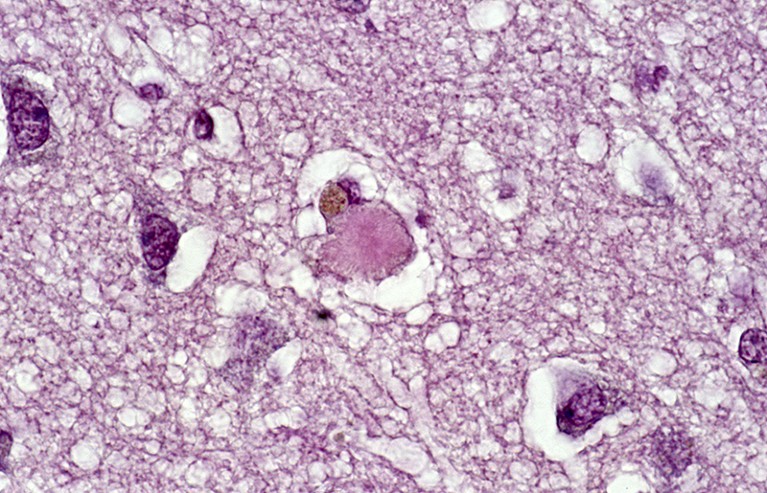
An amyloid plaque (brown) in brain tissue.Credit: PR J.L. KEMENY-ISM/Science Photo Library
Understanding the cause of dementia is also important to determining how to treat it. Although 60–70% of dementia is caused by Alzheimer’s disease, according to the World Health Organization, there are other types that don’t involve amyloid plaques or tau tangles and therefore wouldn’t be helped by these drugs. Memory impairment can also be caused by poor sleep, depression and interactions between prescription drugs. “So just doing cognitive testing and a simple structural brain visualization is not good enough,” says Oskar Hansson, a neurobiologist at Lund University in Sweden. “You need a biomarker that shows if you have amyloid and tau in your brain, and you can’t really do that in any other way except using blood tests, cerebrospinal fluid tests or a PET imaging test.”
One blood test that finds plaques, PrecivityAD, from C2N Diagnostics in St. Louis, Missouri, received breakthrough device approval from the FDA in 2019, so can be requested by physicians. A study in February by Hansson and his colleagues found that the test had a diagnostic accuracy that was similar or superior to that of CSF tests1. A second study by many of the same researchers, published in July, took it a step further2. It evaluated how well the test performed in the conditions found in primary-care settings. That meant that blood samples were collected and sent for testing on a rolling basis, not just for optimized laboratory experiments in which all samples are analysed in a single batch. “I was, to be honest, a bit surprised that the accuracy of a blood test was just as good when we did it that way compared to when we did it the more perfect way,” Hansson says. Hansson adds that this was the first time, to his knowledge, that such testing was studied in a primary-care setting, which is where it might do the most good.
The results were impressive. The combination of two types of biomarker, forms of amyloid-β and tau, gave an accuracy of 90%, as did checking for tau alone. Primary-care physicians had a diagnostic accuracy of 61% using cognitive tests and a computed tomography (CT) scan, and dementia specialists had a 73% accuracy. To achieve that accuracy on the test, the researchers chose a cut-off value for measurement of the proteins. People who came in below that value were judged not to have Alzheimer’s, whereas people above it were considered positive for the disease.
A better approach, Hansson says, might be to choose two cut-off points, which is done with some other types of diagnostic test. People below the lower value would be deemed free of Alzheimer’s; those above the higher one would be positive; and people whose results fell between the two values would be evaluated further, perhaps with a CSF test or a PET scan. When the team used two cut-offs, the predictive value of the test rose to 95% for those who were not in this ‘grey zone’. Doing it that way would limit the more expensive, harder-to-get testing to a smaller subset of people — about 15% of those tested in this study — saving money and reducing stress for individuals, Hansson argues.
Other markers
Other tests to try and differentiate between types of dementia are under development. In 2022, Mayo Clinic Laboratories in Rochester, Minnesota, created a blood test called NFLC for neurofilament light chain, a protein in neurons that increases in the body when neurons are damaged. Although NFLC can indicate the presence of Alzheimer’s, the protein it detects also shows up in other neurological disorders, including multiple sclerosis and motor neuron disease (amyotrophic lateral sclerosis). Still, the existence of a blood test, when before only a CSF test was available, allows clinicians to rule out some possible causes of memory impairment and to monitor the response to treatments in some individuals.
In late 2023, researchers at the University of Oxford, UK, developed a blood test to detect α-synuclein, a protein involved in Parkinson’s disease — the most common neurodegenerative disease after Alzheimer’s — and Lewy body dementia. Parkinson’s disease starts several years before the symptoms of tremors and stiffness appear. Physicians hope that being able to identify the disease earlier will lead to more effective treatments.
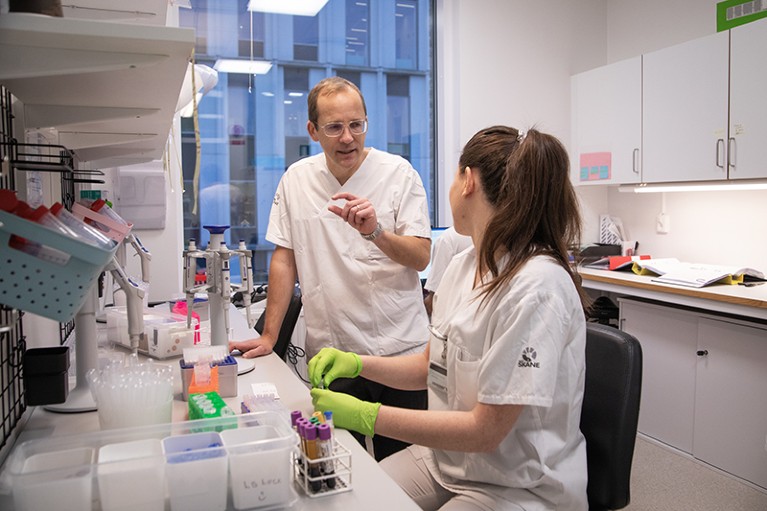
Oskar Hansson and his colleagues have assessed blood tests that find amyloid plaques.Credit: Oskar Hansson
The same could be possible with the Alzheimer’s blood tests. Although they’re aimed mainly at confirming the disease in people who are showing symptoms of cognitive impairment, they are also being used to select individuals for clinical trials. The build-up of amyloid plaques and tau tangles could begin a decade or more before clinical symptoms of Alzheimer’s appear, providing a potential target for new therapies that might interrupt the disease before it progresses. Both donanemab manufacturer Eli Lilly, and lecanemab makers Biogen and Esai, are running trials that look for elevated levels of tau in people who do not show symptoms and test whether their drugs might prevent the disease from progressing.
Many specialists think that such therapies could be more effective if they are started earlier, Hansson says. “If that turns out to be true, one could discuss screening of people at certain ages with genetic risk factors for Alzheimer’s disease, just as we do with prostate specific antigen test for prostate cancer,” he says. The APOE4 gene has been identified as a risk factor for Alzheimer’s, so it might make sense to test people with two copies of that gene — and who are therefore at higher risk of developing the disease — at an early age, perhaps 50, he suggests. Those with only one copy, and therefore medium risk, might be tested at age 60. And people without the gene might start being tested at age 70, when their risk begins to increase. Even five years ago, Hansson says, he would not have thought such screening would be possible, but now he thinks it could arrive in the next decade.
Biological clock
As well as tests to diagnose specific types of dementia, another group of researchers is looking at measuring proteins in the blood to sort people into risk groups for a variety of age-related diseases, including dementia. These researchers created what they call a proteomic ageing clock3. Biological function is a better measure of age than is simply looking at a calendar, the researchers say, and more rapid ageing — measured by the increase of certain proteins — is a strong predictor of diseases such as cancer, diabetes, and liver and kidney problems. “It has a lot of value in predicting who will develop a number of different types of diseases in the future,” says Austin Argentieri, a public-health researcher at Massachusetts General Hospital in Boston. “It just so happens that the disease that it’s most strongly associated with is Alzheimer’s.”
Argentieri and his colleagues looked at data for more than 45,000 individuals recorded in the UK Biobank, a collection of genetic samples and health records. They examined measurements of nearly 3,000 proteins in the blood of those individuals and used machine learning to sort out how protein levels correlated with the development of disease. It turned out that blood levels of a collection of 204 proteins strongly predicted what diseases people would be diagnosed with 10–15 years later. That’s not surprising, Argentieri says. “What ageing really entails is kind of an accumulation of biological changes over time,” he says. “Those same biological changes, at least in terms of the proteins, are the ones that are ultimately causing disease.”
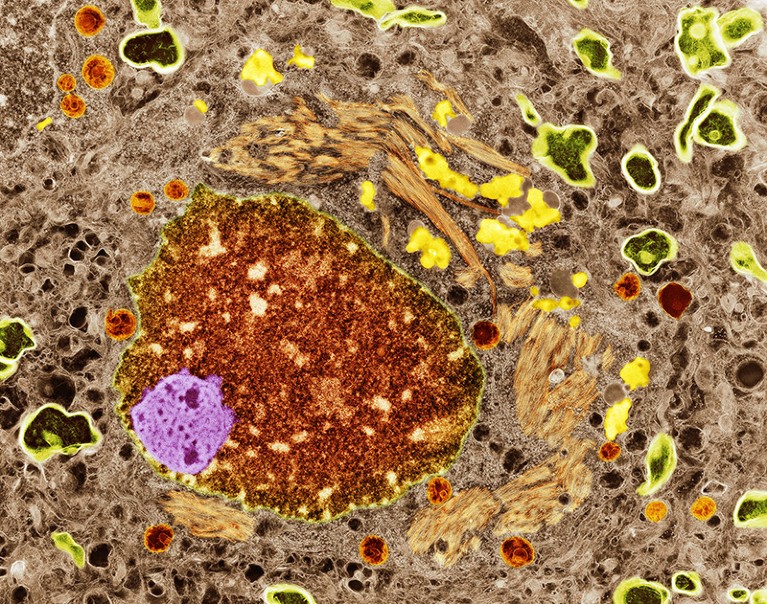
Tau-protein aggregates (orange) are found in people with Alzheimer’s.Credit: Thomas Deerinck, Ncmir/Science Photo Library
The researchers sorted people by the gap between how old they were chronologically and how old the protein measurements said they were. The difference between the top 5% of the sample — who were ageing more rapidly than their years might suggest — and the bottom 5% was about 12 years, and the top 5% had an Alzheimer’s risk almost six times that of the bottom 5%. The risk for all causes of dementia was also higher for those who were ageing the most rapidly, although the sample was too small to tease out individual types of dementia other than Alzheimer’s.
Argentieri stresses that the proteomic clock is not a diagnostic tool for any particular disease but rather one for predicting risk. That could allow people with higher risks to take steps, such as lifestyle changes or possibly medication to change their risk levels. The hope, he says, is that “you can put yourself on a very different future trajectory of what your health and well-being might look like”.
Ditz is trying to manage his own trajectory with Alzheimer’s after getting through the initial emotional turmoil of finding out he had the disease. He’s taking the drug donepezil to treat his symptoms. He has also joined a support group, is trying to stay socially engaged, eats well and has stopped consuming alcohol. He also has a one-year appointment to the early-stage Alzheimer’s group of the Alzheimer’s Association in Chicago, Illinois, where he tries to help others by sharing his experience with the disease.
He thinks that having a blood test that is cheaper, faster and easier than the process he went through will help a lot of people. “It really does feel a little bit like magic or an incredible short cut to get you to a real answer,” he says.
And he thinks that science is close to changing the course of the disease. He attended a meeting a few months ago with speakers from the research community. “They were starting to use the word ‘cure’ as something that’s really attainable and not just a myth or a hope,” Ditz says. “That kind of helps us to feel optimistic and to do our bit, and make our children and grandchildren not have to worry about this.”



